Neurophysiologic Intraoperative Monitoring With Sugammadex
Let me start off by saying this… I have no experience with the use of Sugammadex during neurophysiological monitoring. The drug was denied FDA clearance in the USA in 2008, so maybe some UK readers can chime in and help out with their experience.
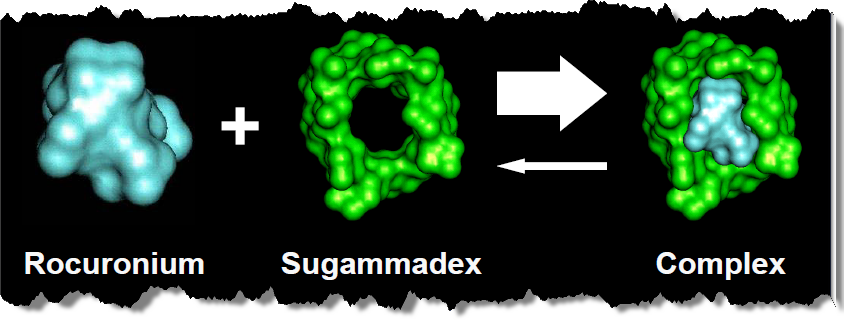
Sugammadex is used to reverse rocuronium without the need of any twitches. And from what I’ve read, it seems like it would be a nice option to have. With the use of nerve and pedicle screw stimulation and motor evoked potentials increasing over the years, this could make intraoperative neurophysiological monitoring even easier and safer.
7 instances where Sugammadex might be of benefit…
- If you are monitoring a cervical trauma case, you’ll want prepositional baselines while anesthesia wants an easy intubation without needing to extend the patients head. Here, you could set up SSEP for preintubation baselines, anesthesia could give the patient rocuronium for intubation, reverse them to get MEP baselines, and then position the patient. Unlike current reversal agents (acetylcholinesterase inhibitors, e.g. neostigmine), sugammadex can reverse profound blockade and can be given for immediate reversal without the need to wait for partial recovery.
- I just wrote about the difficulties in neuromonitoring obese patients, but anesthesia has some things to worry about too. Complete and fast recovery of neuromuscular function is very important in morbidly obese patients because of the possible influence of postoperative residual curarization (PORC) on respiratory function in the postoperative period. Administration of sugammadex provides fast recovery of neuromuscular function and prevents PORC in the morbidly obese, however, neostigmine does not. http://www.ncbi.nlm.nih.gov/pubmed/22012861 The availability of sugammadex 16 mg/kg to reverse immediately block induced with high-dose rocuronium means that rocuronium + sugammadex could be considered as a replacement for succinylcholine for rapid induction (and reversal) of NMB.
- A case where you are running MEPs, but the patient requires rapid sequence induction of anesthesia for endotracheal intubation, the immediate reversal possible with sugammadex could enable large doses of rocuronium to be used in the knowledge that should a ‘cannot intubate–cannot ventilate’ situation occur, then the blockade will be reversible. Use of sugammadex in this setting would avoid the potentially serious adverse effects of the currently used agent, succinylcholine, including anaphylactic/allergic reactions, cardiac arrest, myalgia and inducing malignant hyperthermia. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0014971/
- Neuromonitoring reimbursement isn’t the only ones getting slashed. Cost is a big issue with all of healthcare right now. In the routine setting, under the base-case assumptions, 2 mg/kg (4 mg/kg) sugammadex appears cost-effective for the routine reversal of rocuronium-induced moderate (profound) blockade at the current list price (2 ml × 10 vials,£596.40; 5 ml × 10 vials, £1491.00; 100 mg of sugammadex per millilitre) if all reductions in recovery time associated with sugammadex are achieved in the operating room, but does not appear cost-effective if all reductions in recovery time are achieved in the recovery room. Where savings in recovery time are achieved in both the operating room and the recovery room, or where there is additional value in reducing recovery times (for example in preventing operations from being delayed or forgone), the cost-effectiveness of sugammadex is highly dependent on the setting in which it is administered. Of course, further study is needed to see if it helps reduce cost with neuromonitoring (from decreased morbidity, decreased surgical time, etc.)
- The main advantage of sugammadex is reversal of neuromuscular blockade without relying on inhibition of acetylcholinesterase. Therefore it does not cause the autonomic instability produced by anticholinesterases such as neostigmine, and antimuscarinic agents such as atropine do not need to be co-administered. Its administration is therefore associated with much greater cardiovascular and autonomic stability than the traditional reversal agents. A very nice benefit to have if used with MEPs during vascular cases.
- When neuromonitoring is used, baseline MEPs are important because by comparing them with all motor responses that follow, we can identify neurological problems. Patients should be completely reversed from muscle relaxation in order to perform accurate neuromonitoring (MEPs) from the beginning of surgery. Even 50 mins after rocuronium administration there was a decreased response to MEPs for some patients. http://journals.lww.com/ejanaesthesiology/Fulltext/2012/06001/Sugammadex_administration_improves_neuromonitoring.337.aspx
- If a wake-up test is ordered by the surgeon, the patient needs to be able to move… pronto. Despite the wide variability, reversal of the TOF ratio to 0.9 occurred < or = 5 min in more than 80% of the patients regardless of the number of twitches at the time of reversal drug administration. It’s just fast.
- **Bonus reason** – Some surgeons want complete paralysis till it is time to test pedicle screws. Sugammadex would be a nice option to make sure you have 100% reversal within a short period of time.
And I’m sure you can think of plenty of other instances where Sugammadex might be of use. I’d like to see it get clearance in the States. And I know the anesthesiologist and CRNA’s I work with would love it too.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...







Or, reason #8- When the anesthesia resident spaces out and gives Roc because she forgets you’re monitoring MEPs.
I wonder why it was not approved in the US. Does anyone know? Does it only work with rocuronium?
http://www.drugs.com/history/sugammadex.html
Dear Joe
I wonder if you can tell me where you got the image of sugammadex encapsulating rocuronium as I would like to use it myself?
Many thanks
Ciara