Everyday Neuromonitoring With Anesthesia Conversations…
Everyone has their own experiences working with anesthesiologist and CRNAs. At some facilities, the neuromonitoring clinician tells the anesthesia team what they need, and anesthesia accommodates. At other facilities, neuromonitoring with anesthesia takes some negotiation.
Win some, lose some.
But a lot of the same conversations happen over and over. It makes sense to have simple, well thought out responses to these questions.
Before we get into the conversations you have to have before a case, let’s go over some simple things you can do in order to avoid the conversations you don’t have to, or want to, have with anesthesia.
- Be part of the team. We are all there for the patient’s best interest. If there is some conflict in what is needed for monitoring and what anesthesia is able to deliver, always remember to keep the rest of the team in the loop. Both the anesthesia and the surgical team needs to be in on the conversation. They need to know going in what your confidence level will be in the data being collected. They will usually either tell you thank you for the heads up or further discuss the anesthesia plan.
- You are not an anesthesiologist (unless you are). You can not tell them what to run. You can only make recommendations on what the surgeon has requested you to do and what you need from them in order to achieve it. There usually is no problem, but not always. Anesthesia has many things to consider (bone density, cardiac integrity, liver and kidney issues, etc.). We tend to jump to the conclusion that they are either being lazy or are incompetent if they can’t do what we ask. There might be much more to it than we know.
- Know how to give suggestions. If anesthesia blatantly ask you what to run, doses, etc., you are best to phrase it as “I have worked with other anesthesiologists who have done XYZ, does that work with that you need to accomplish?” or “I’ve seen in the literature, I’ve seen XYZ used successfully, would that work with what you need to accomplish?” We are not prescribing anything, just telling from the experience of working in the operating room or read in journals.
- Have the conversation early. Give anesthesia as much time to get set up as you can by finding the surgeon and verifying what type of monitoring they would like. They hate it when you tell them you need something that requires a pump that they don’t have in the room.
- Give them space. Their job is to keep the patient unconscious, without pain, without memory, without movement, with stabilized vitals and alive. In a time of crisis, they need to move fast. Always try to keep your wires under all of their stuff and needles well secured. It is less likely to get pulled out and they can work without having to deal with a tangled mess.
- Keep an eye out. It helps to be able to see what the anesthesia is running and what vitals look like before and during the case. This will help you rule in or out any issues that might arise. Get a good seat in the OR, or see if you can get it put up on a TV screen in the room.
- Don’t be a pushy jerk. You’ll piss everyone off and eventually, all your request will get shot down.
- Don’t be a pushover. You think you’re playing nice, but you’ll eventually get in the position where you won’t be able to monitor due to anesthetic effect. The surgeon is going to be upset at both you and the anesthesia team for not working it out beforehand.
Having a good working relationship with anesthesia makes your job much easier. The daily conversations that you have with them tend to go much smoother.
Here are the quick and dirty protocols that you need to know. Of course, this isn’t the only way to get things done. This list is the bare minimum but will get you through a very high percentage of your cases.
The Key:
The list is by what modality you are going to utilize.
What you say to anesthesia is in quotes.
What anesthesia might say back is in Italic.
Spine correction cases
- Only EMGs
- “Go ahead and use any gas or nitrous, I just need the muscle relaxant to wear off after exposure.”
- So how long should I paralyze the pt?
- “I’m not sure how long the surgeon is going to take for exposure, let’s ask him/her.”
- Short-acting or minimal dose of muscle relaxant for percutaneous surgery.
- So how long should I paralyze the pt?
- “Go ahead and use any gas or nitrous, I just need the muscle relaxant to wear off after exposure.”
- SSEP only
- “You can use mm relaxant throughout the case, with half a MAC of gas, up to a MAC if needed and no nitrous” (side note: 1 MAC of inhalant is usually OK to maintain SSEPs, but if you say that can use a MAC, they will use that as the lowest level).
- Why can’t I use any nitrous?
- “When nitrous is combined with other inhalants it really diminishes my waves, then I can’t tell if there was some neurological problem or if it was due to anesthesia.”
- Why can I only use a MAC of gas?
- “When inhalants are too high it really diminishes my waves, then I can’t tell if there was some neurological problem or if it was due to anesthesia.”
- Why can’t I use any nitrous?
- “You can use mm relaxant throughout the case, with half a MAC of gas, up to a MAC if needed and no nitrous” (side note: 1 MAC of inhalant is usually OK to maintain SSEPs, but if you say that can use a MAC, they will use that as the lowest level).
- SSEP and EMG
- “You can use mm relaxant through exposure, with half a MAC of gas, up to a MAC if needed and no nitrous.”
- Short-acting or minimal dose of muscle relaxant for percutaneous surgery.
- “You can use mm relaxant through exposure, with half a MAC of gas, up to a MAC if needed and no nitrous.”
- SSEP and MEP
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation. Oh, a bite block too, please.”
- So I can’t use any inhalant/nitrous?
- “The motors are really sensitive to anesthesia and it will knock out my waves”.
- Well, what can I use then?
- “I’ve seen other anesthesiologist use around 120mcg/kg/min of propofol with remifentanil.”
- I can’t run this case on just propofol and remifentanil, I have to use something.
- “OK, let’s talk to the surgeon to see what he/she wants to do knowing that this person can’t be run on TIVA protocol.”
- What kind of muscle relaxant can I use to intubate?
- “Succinylcholine.”
- I can’t use that on this pt because….
- “That’s OK. You can use something that is usually a little longer lasting but try to use an amount that will wear off in 15 minutes once you start your intubating. I’ve seen other doctors use 20 of rocuronium with good results. It will take me that long to get my leads all set up, so it should work out OK.”
- I need them paralyzed to position.
- “OK, let’s talk to the surgeon and see what he/she wants to do knowing this. I believe he wants postpositional SSEP and MEP.”
- I can’t use that on this pt because….
- “Succinylcholine.”
- I’ve read that I can use gas when doing motors, why are you telling me that I can’t?
- “The paper that most people reference is the one done by Todd Sloan where he uses .25 MAC. Our company had a meeting on this issue and everyone agreed that some cases do fine with .25 MAC, but there is still a decent percentage of people will lose motors. It seems to slowly decrease the amplitudes over time till they just disappear. And because I can only run them periodically, I might not be able to tell it is happening till it is too late. At that point, we can’t tell for sure if it is an anesthetic issue or something else. It’s been reported in the literature that it can take 40 minutes to recover MEP responses after the gas is shut off.”
- I talked with the surgeon and s/he said that if I need to use gas that I should.
- “Thanks for doing that… I’ll let you know how things are going during the case and we can go from there.”
- Is any of the gasses better than the others for motors?
- “Yes. Please use Des if you can. It seems to work less on the alpha motor neurons than the other inhalants and doesn’t hang around as long should we need to shut it off.”
- So I can’t use any inhalant/nitrous?
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation. Oh, a bite block too, please.”
- SSEP, EMG, MEP
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation. Oh, a bite block too, please.”
Cortical Mapping
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation. Oh, a bite block too please.”
- Same conversations as with MEPs.
Phase Reversal
- “You can use muscle relaxant throughout the case, with half a MAC of gas, up to a MAC if needed and no nitrous.”
- Same conversations as with SSEPs.
Phase Reversal and Cortical Mapping
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation. Oh, a bite block too please.”
- Same conversations as with MEPs.
- “Use muscle relaxant throughout the case, 1 Mac of inhalant, no nitrous, and a low dose of remifentanil so there is no burst suppression on EEG.”
- I’d like to use propofol too. How much propofol am I going to need to get keep them from burst suppression?
- “It is different for every person, but adding propofol on these has caused problems on EEGs in the past. I’ve had other anesthesiologists start at around 35-70 mcg/kg/min. If you have to use it, we can see how things go from before exposure of the carotid. We need to figure out a good steady state 10 minutes before clamping so I am confident that any burst suppression seen is due to lack of blood supply and not anesthesia.
- I can only use 1 MAC of gas?
- “I am running SSEPs as well. Anything over that will start to decrease my amplitudes.”
- I’d like to use propofol too. How much propofol am I going to need to get keep them from burst suppression?
Aneurismal Clipping
- “Use muscle relaxant throughout the case, with half a MAC of gas, up to a MAC if needed and no nitrous. Please have a propofol pump ready with enough to cause burst suppression during the clipping.”
- How much propofol am I going to need to get them into burst suppression?
- “It is different for every person. I’ve had other anesthesiologists start at around 120mcg/kg/min. We’ll see how things go from there. We need to figure out a good steady state 10 minutes before clipping so I am confident that there is good neural protection.”
- I can only use 1 MAC of gas?
- “I am running SSEPs as well. Anything over that will start to decrease my amplitudes.”
- How much propofol am I going to need to get them into burst suppression?
- “TIVA protocol (total intravenous anesthetic protocol) with some kind of short-acting mm relaxant up front for intubation.”
- Same conversations as with MEPs.
- “Don’t worry about those, anesthesia won’t affect them much at all.”
- Just use protocol for whatever else you are running in that case.
Dorsal Column Topography (recording cortical SSEP from spinal cord stimulation)
- “You can use muscle relaxant throughout the case, with half a MAC of gas, up to a MAC if needed and no nitrous.”
- Why can’t I use any nitrous?
- “When nitrous is combined with other inhalants it really diminishes my waves and I won’t be able to tell where they are in the spinal cord.”
- Why can I only use a MAC of gas?
- “When inhalants are too high it really diminishes my waves and I won’t be able to tell where they are in the spinal cord.”
- Why can’t I use any nitrous?
- As needed for other modalities.
Dorsal Column Topography (recording a peroneal nerve from spinal cord stimulation, or stimulation of peroneal nerve and record over the spinal cord).
- As needed for other modalities.

Joe Hartman
Subscribe to our Awesome Newsletter.
1 Comment
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Run Hypoglossal Nerve Stimulation For Obstructive Sleep Disorder
Hypoglossal Nerve Stimulation: A Novel Technique for IONM This isn't our first time helping surgeons map out nerves. We are starting to see some traction in hypoglossal nerve stimulation for obstructive sleep apnea. Obstructive sleep apnea is one of the most prevalent...
How To Avoid An Unimpressive IONM Resume…
What Does Your IONM Resume Say About You? Let's break down the neuromonitoring field a little bit here (it will help your IONM resume not suck)... If you had to guess what percent of the cases your company monitors are spine cases, where would you place your bets? If...
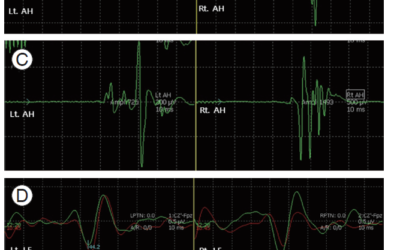
Changing My Mind on TIVA For Carotid Endarterectomy?
Beliefs Are Identities In hindsight, it was obvious. It almost always is. But this one seems like a real head smacker. I don't need any modern equipment; 30 minutes and a playground and my 2 boys will make a bulletproof case for handwashing. Their fingernails will...
IONM Conferences Are Back! Here’s How to Make the Most of It…
Remember a couple of years ago when we would all meet up at IONM conferences to share ideas and network in real life? Well, I'm venturing off to my first one since COVID-19 hit. This year's ASNM annual meeting is in Clearwater, Fl on May 20th and I'll be there looking...
The Thing I Wanted Most For IONM: Improved Signals In Spine Surgery…
Signal Improvements In tcMEP and SSEP During Spine Surgery What does everyone want for IONM? Needless recording electrodes and cordless monitoring equipment. Both would be great -- if it actually worked like the alternative. But I can't be alone in thinking this:...
It’s NOT Motor Mapping Vs. Navigation; It’s Motor Mapping And Navigation…
The surgeon uses navigation and wants to know why she should use motor mapping for her crani? That's the question posed to me by a clinician years ago. It was just before I set up my case and they recruited me into the conversation. So I walked over to the room next...
Help Spread The Word. Social Media Works!




Great Cheat Sheet!
You appropriately listed as 1. Be a part of the team, so important for dialogue between surgeon, anesthesia and neuromonitorist to keep the patient’s best interest foremost in all parties’ minds.
When I worked In-house I would give brief Power Point presentations to the Anesthesia staff on the various types of monitoring required , very much like what you presented. I would show them slides of cases where the gas used severely affects the meps and now as a traveler I show them nicely on the screen when using even a small amount of gas what effects. Usually with your strategy above most times we get the anesthesia that best serves the patient. But as you know unfortunately, there are some in anesthesia that have been misinformed or misunderstand for some reason or another.