Here’s the reality for people that want to get trained on doing d-wave and dorsal column mapping on spinal tumors… you most likely aren’t going to have the luxury of seeing 30 of these before you start doing these yourself.
Unless you are the exception and work at a facility that just knocks these out, you’re not going to get too many of these requested. That means that you’re going to have to go in with a firm understanding of overall neuroanatomy and neurophysiology and be able to apply that knowledge to the case in front of you.
These are very high-risk surgeries where neuromonitoring and mapping play a crucial role in the surgical planning and outcomes. Please do not attempt these cases if you’re experience level is not yet there.
A Mock “In-OR” Experience
It’s difficult to provide operating room experience from outside the operating room. You really need to be in there to train appropriately.
That being said, there are ways to prepare that will shortcut your learning curve. Part of that is going through textbooks and research articles, but there is more to it than that.
One thing that helped me be able to quickly broaden my scope of neuromonitoring cases quickly was to look a the company schedule and prepare for every case we had on the board for that day. Here’s what that exercise would look like:
- make a list of what modalities I would run
- list out all supplies I will need
- write a program for the case if I didn’t already have one
- mentally go through the IONM setup
- mentally go through the surgical case
- try to predict the conversions I would have with anesthesia and the surgeon as it pertained to that case
- determine the parts of the surgery with higher risk and what modality would be affected
- alarm criteria for each modality as it pertains to that procedure
- common technical problems that could happen and how to troubleshoot them
- write a case note
It took forever to do it, but I really think it cut my learning curve down significantly. There’s only so much you can learn at one time, so instead of asking Day 1 questions on Day 1 (like “what modalities should we run for this case?”) I was able to jump ahead of schedule.
Even though you might not see a D-wave and dorsal column mapping case on the schedule often, you should still go through the process. So that’s what I’m going to do here. (Going through these mental exercises is where I found it useful to take the position of different people in the OR, which is why I use the cartoon characters on my presentations and this website.)
Case: Cervical Intramedullary Tumor
Here we are going to walk through the case from the night before till the end of the case as it is likely to play out. Conversations between the surgical neurophysiologist, the training neuromonitoring technician, the anesthesiologist and the surgeon are shown next to the cartoons.
- bilateral ulnar nerve
- bilateral median nerve
- bilateral posterior tibial nerve
- bilateral Erb’s point
- bilateral popliteal fossa
- FPz
- CPz
- CP3
- CP4
- Cs2
- Ground
- M1 tcMEP
- M2 tcMEP
- bilateral trapezius
- bilateral deltoid
- bilateral bicep
- bilateral triceps
- bilateral first dorsal interosseous
- bilateral tibialis anterior
- bilateral abductor hallucis brevis
- d-wave reference electrode
If the cervical tumor is located below C6, I might elect to get rid of the trapezius (control) and add another lower extremity muscle for redundancy (extensor digitorum brevis). The deltoid would then be my control for tcMEP.
All I need to do is remember to bring a concentric bipolar probe and 2 spinal recording electrodes for d-waves.
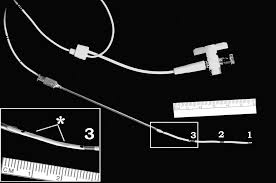


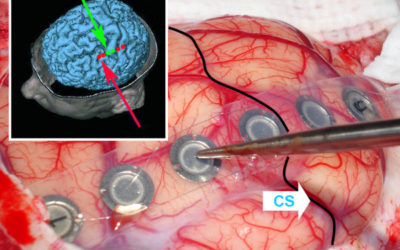
The spinal recording electrode (on left) is meant to be placed on the spinal cord for d-wave recording. The surgeon can place it either epidural or subdural. They should use 2 electrodes for the procedure. The first should be placed rostral to the surgical area, with the tip going up towards the head. The second one should be placed caudal to the surgical area with the tip going towards the feet. The surgeon can then secure both with a loop tie.
You’ll notice some other items in the box. There is a needle and tubing for fluid if you were going to place the electrode percutaneously. I personally have never done percutaneous d-wave monitoring. I would image it to be pretty difficult to get something reproducible.
Don’t let the concentric bipolar probe fool you. It looks like a monopolar probe at first. But it is, in fact, a bipolar probe. You will plug the anode and cathode into your stimulator box and do not have to worry which goes where. No reference needed, like when using a monopolar probe.
If you were using a bipolar probe, then you would need to make sure the cathode is position correctly, depending on the dorsal column mapping technique you’re planning on using. You also need to monitor the surgeon to make sure they have the probe position correctly. The concentric probe eliminates this need and provides a very localized stimulation. Both are very useful when stimulating over such a small area.
Writing The D-Wave And Dorsal Column Mapping Program
Since the D-wave recording electrodes have 3 channels, it gives you 3 opportunities to record a response. In the rostral electrode, you will want to reference 1-2, 2-3, and 1-3. When recording the traces, you can elect to use the best one or 2 to monitor. Since the caudal electrode is facing the other direction, you’ll want to reverse your active and reference electrodes so that you get the same negative response to monitor off of. That would be 2-1, 3-2 and 3-1.
I would also recommend having a reference electrode placed beforehand in case of an emergency. Say you’re unable to get a bipolar response for some reason. It only cost you 1 electrode to test out a referential response, say 1-ref, 2-ref or 3-ref. If you’re using something less user-friendly, like the eclipse, try to have it programmed ahead of time. If you’re using a program where changes on the fly aren’t a big deal, like the Cadwell, you may elect to not have it preprogrammed if you’re running short on channels.
Stimulating a D-wave should be setup exactly like a tcMEP with 1 major exception. Because we are only recording the direct cortical activity from the lateral cortical spinal tract we do not have to worry about synapses. This means that having multiple train impulses is unnecessary. This allows us to stimulate without any patient movement and allows for continuous monitoring. But you’ll be able to use the same M1/M2 electrodes you’re using for tcMEP.
The amplitude is somewhere around 5-50uV. With an amplitude that large, it should have a pretty good signal-to-noise ratio. You’ll still want to set up some sweeps (5-20) to make sure that the amplitude you’re measuring is really representative of the conduction along the lateral cortical spinal tracts.
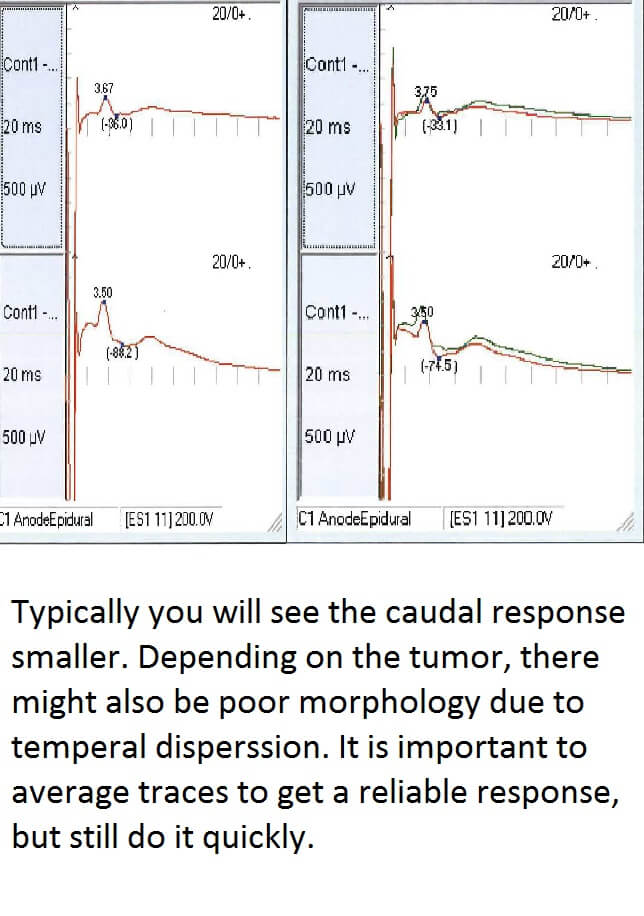
When setting up the filters, a low-cut of 100, a high-cut of 5,000 and a gain 200 of have worked for me.
As far as stimulation intensities, it is going to be less than what is used to elicit a compound muscle action potential in the limbs when using a multi-pulsed tcMEP. What you’re looking to achieve is the largest D-wave amplitude without causing the patient to move. That way you know that you’re monitoring most of the fast conducting fibers along the lateral cortical spinal tract.
As you move up in intensity, you’ll notice the onset latency of the response will decrease. This is most likely due to the fact that the higher intensity will cause deeper stimulation, which will shorten the length the potential will have to travel.
Dorsal column mapping is relatively easy to do from a programming standpoint. You are going to set up a stimulator through a probe for an evoked potential, just like you would for an SSEP. Since the stimulation is directly over the spinal cord, you can use much less power in order to evoke a response. At 3.11 Hz, a pulse width of 200us and starting at 0.2mA, you should be able to get a response below 2mA. In fact, you want the intensity low enough to get a reliable response, but not high enough to cause current spread.
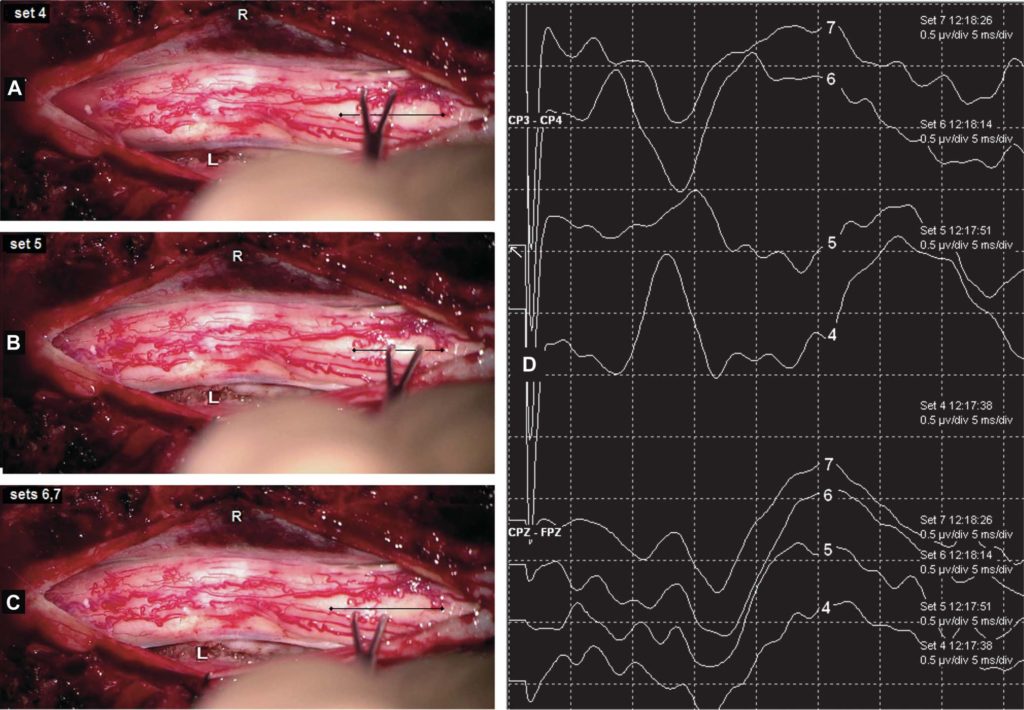
The cortical channels you’re going to use is CPz-CP4, CP3-CP4, CPz-FPz, CPz-CP3, and CP4-CP3.
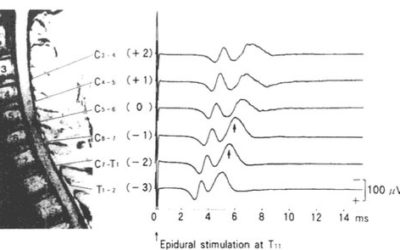
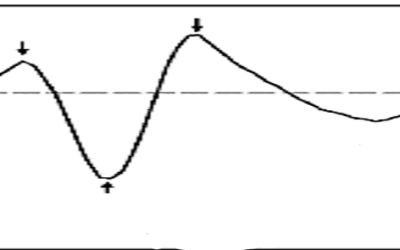
When stimulating over the left dorsal column (just like when stimulating over the left posterior tibial nerve) you’ll see a P40 response (which will actually be much shorter than 40ms) on CP3-CP4 and CPz-CP4, with phase reversal at CP4-CP3 and CPz-CP3. The opposite pattern will be seen when the surgeon stimulates over the right side of the cord.
CPz-FPz will always show a P40 response unless the surgeon is directly over the dorsal median sulcus. If this is the case, you should see an isoelectric response from all cortical channels. That is the anatomical area the surgeon will want to enter. You can see the phase reversal below in the CP3-CP4 channel from #4 (left dorsal column), #5 (dorsal median sulcus) and #6 (right dorsal column).
Is TIVA Needed For D-Wave Monitoring?
Here we really need to discuss what is best for the patient. We need to be able to really rely on tcMEP as they match up with D-wave recordings in order to best assess this patient throughout the case. This is one of those cases where you really need to work hard to get TIVA with full 4/4 during the time of laminotomy. While you don’t need TIVA to get D-waves, you need TIVA in order to best compare your motor evoked potentials to D-wave recordings. You’re going to want to make sure that you have as reliable of tcMEP at that time as you possibly can. While the aesthetics will not really affect the D-wave monitoring, and only affect the mapping as much as it would SSEPs, we need to make sure we have optimal tcMEPs. (We will get into why later when we talk about alarm criteria).
For cervical tumors, these patients will often times have a positive Lhermitte’s sign, weakness, loss of sensation and other spinal cord injury signs and symptoms. You’ll want to do prepositional baselines for SSEP and tcMEP. You’ll want to see if the anesthesiologist is willing or able to intubate without muscle relaxation. If not, then they need to use very little or something short acting.



The concentric bipolar goes into our stimulator box and the 2 spinal recording electrodes go to the pods or amp. You showed me the phase reversal in dorsal column mapping, but can you go over the alarm criteria for D-waves now?
D-Wave Alarm criteria
The best way to use reduction of D-wave amplitude is to compare it not only to the baseline measure but also against tcMEP responses.
- If D-wave <30-50% + mMEP stable = No deficit
- If D-wave <30-50% + mMEP lost = Transient deficit
- If D-wave > 50% + mMEP lost = Permanent deficit
- Any decrease in D-wave should be reported
This is important information for the surgeon to know. If the tumor is one that has great outcomes with complete removal, then the surgeon might elect to continue with tumor resection with lost tcMEP and D-waves with minimal reduction. If they remove the tumor and have a transient weakness, that’s a victory.
But if the tumor isn’t in this class, then the surgeon might elect to stop tumor removal in order to preserve function. This might happen in cases where the life expectancy is not too long. The patient might choose to have motor and sensory function in their last days over getting all the tumor.
Troubleshooting Dorsal Column Mapping
- The surgeon needs to make sure they are absolutely still while placing the probe on the spinal cord.
- The stimulation intensity needs to be low enough to collect a response and not cause shunting
- CSF needs to be suctioned out and the surface dried off
- Take your time with the initial baselines to get optimal responses. This might mean testing out CP1 and CP2 also.
- Be able to try out other ways to perform dorsal column mapping
Troubleshooting D-wave Monitoring
- Check impedances. Poor contact with the spinal cord can be a reoccurring problem. You may never get great impedances.
- Surface electrodes get noisy. You might have to play with your filters to get rid of noise and/or stim artifact. Do not let the changes in latency fool you. It will happen.
- If you stimulate too high, muscle artifact from the paraspinal muscles can be seen. This should be later than the typical response latency. You might get it regardless in the cervical spine.
- Latency is around 2-3 ms in the cervical spine and 9-10 ms in the thoracic spine. The lower you go, the longer the onset latency. The higher you stimulate, the shorter the onset latency.
- Do not place your ground in the head. Not a good move whenever stimulating transcortical.
- Use a referential montage if you can’t get a bipolar response.
In-House Or Contractual Neuromonitoring Company: Where To Work?
IOM Jobs: In-House Or With A Contractual Neuromonitoring Company: Pros And Cons With the amount of people looking to get into neuromonitoring, and some of the larger companies slowing down their hiring till the dust settles on these billing issues, it seems like most...
Neuromonitoring Job: Preparing For The Interview
Interviewing For A Neuromonitoring Job If you got the call for an interview for a neuromonitoring job, then you've already wowed them with your killer IONM résumé. Now comes the part that everyone love... selling yourself without sounding like a braggart, and then...
Direct Motor Evoked Potentials Using Surface Electrodes: Pros and Cons
Direct Motor Evoked Potentials Continuing on from the post about intraoperative monitoring for gliomas (and trying my best not to ramble on too much in this post), I'd like to discuss some pros and cons to using a surface electrode strip as an anode directly on the...
7 Reasons To Love Sugammadex For Neurophysiological Monitoring
Neurophysiologic Intraoperative Monitoring With Sugammadex Let me start off by saying this... I have no experience with the use of Sugammadex during neurophysiological monitoring. The drug was denied FDA clearance in the USA in 2008, so maybe some UK readers can chime...
Variability In Somatosensory Evoked Potential Test: Summing It Up
Somatosensory Evoked Potential Test Variability In my previous 2 post about temporal dispersion and somatosensory evoked potential test variability, I went over how to ID trial-to-trial variability, how to handle it and what was happening to the waveform. I'm going to...
Follow Up Post: SSEP Increased Variability vs. Increased Latency
SSEP Increased Variability vs. Increased Latency: A question from a reader... In my last post, I talked about using the waterfall function to better determine your SSEP baselines, as well as how using it can be helpful in determining your level of confidence with the...



Thanks Joe. Very informational.
Good stuff, thank you!
Thank you for reading.
Why do you use first dorsal interosseous over the more standard thenar/hypothenar?
Personal preference. I have no objective measures that it is better or worse for things like tcMEP or EMG, just my own experience. I know that it is easier to replace in that muscle if something gets pulled when the arms are tucked (like in an ACDF). They are also out of anesthesia’s visual field when they are placing their lines and that has slightly cut down on some of the comments from them. If I suspected compression/stretch of the ulnar nerve (you see this a lot with older women with large Q angles at the elbow) or have some other clinical reason to not use it, then I will use the thenar.