Hypoglossal Nerve Stimulation: A Novel Technique for IONM
This isn’t our first time helping surgeons map out nerves. We are starting to see some traction in hypoglossal nerve stimulation for obstructive sleep apnea.
Stimulating Cranial Nerve XII
For most of us with a little bit of time, providing the IONM service for this sleep apnea surgery will feel comfortable. We’re pretty good at stimulating cranial nerves, recording potentials, and troubleshooting.
The surgery itself might be new to us, so I’ll include some ancillary information to help better understand the goal and pitfalls of the surgery.
But before you go do one of these, like any other new surgery, make sure to watch the surgery being done on Youtube to better orient yourself as to what the surgical cadence and moments of risk to neural structures might be.
What is the hypoglossal nerve?
The hypoglossal nerve starts in the medulla oblongata and travels down through the spinal cord before coming back up again over the tip of the chin.
The tongue muscles need to be strong enough to help them perform their functions of moving our tongues and swallowing.
When this doesn’t happen, those muscles can become lax and close off our windpipes.
We can break these muscles down into extrinsic and intrinsic muscles.
The extrinsic muscles innervated by the hypoglossal nerve
Innervated by the medial division of CN XII
– Genioglossus horizontal pulls the tongue out.
– Genioglossus oblique pulls the tongue down.
Innervated by the lateral division of CN XII
– Styloglossus retracts and elevates the tongue.
– Hyoglossus retracts and depresses the tongue.
The intrinsic muscles innervated by the hypoglossal nerve.
Innervated by the medial division of CN XII
– Inferior longitudinal medial shorten the tongue and curls the tip inferiorly.
– Transverse narrows the tongue.
– Vertical flattens the tongue.
Innervated by the lateral division of CN XII
– Superior longitudinal shortens the tongue and curls the tip superiorly.
– Inferior longitudinal lateral shortens the tongue and curls the tip inferiorly.
What is Hypoglossal Nerve Stimulation Therapy for Sleep Apnea?
Placing a permanent hypoglossal nerve stimulator is an alternative to the gold standard, the CPAP (continuous positive airway pressure) therapy. While the success rate for CPAP is really high, it’s not easy to stick to.
And we know how patients are when it comes to following through with medical instructions. And because of this, there is a 0% success rate in patients that don’t use their CPAP.
So surgery is another option for those not excluded (<18 years old, BMI<32, won’t use the CPAP or isn’t getting consistent results, has bad sleep apnea as defined by AHI range of 15–65 per hour, no retropalatal collapse).
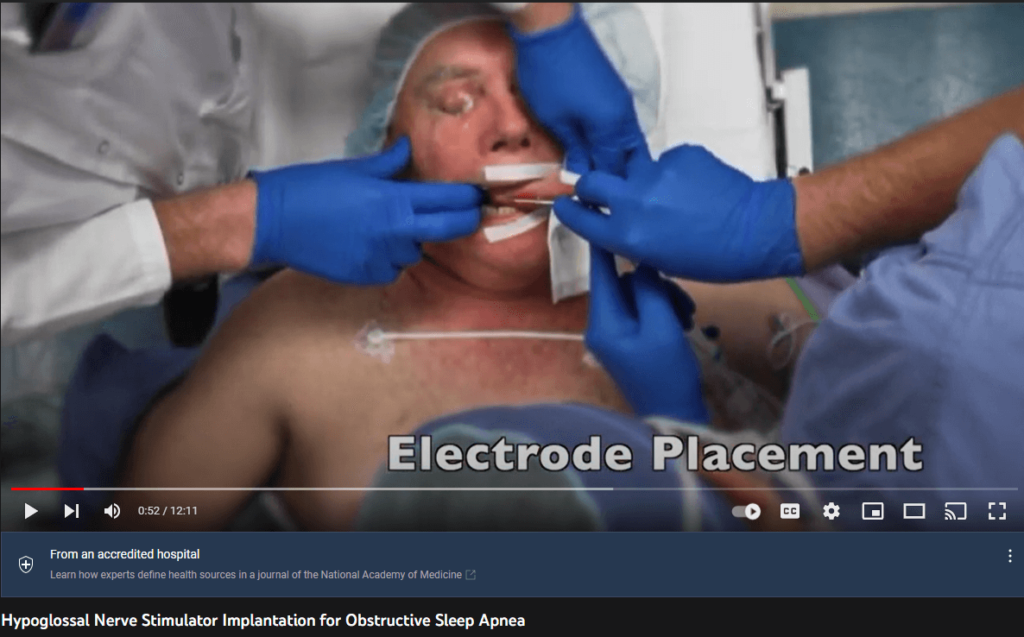
This pretty new surgery is sometimes called the “pacemaker for the tongue” to patients. There is a cuff placed to stimulate the nerve and a sensory lead to detect different pressures. A battery and pulse generator is placed outside the chest (infraclavicular) like we’ve seen in other patients we encounter with pacemakers or spinal cord stimulation devices.
What it does is causes periodic tone in tongue muscles through exogenous stimulation of the CN XII. When relaxed, those muscles can obstruct the airway.
The 2 companies with products we work with (that I’m aware of) are Imthera (LivaNova) and Inspire (Inspire Medical Systems).
Neuromonitoring for Hypoglossal Nerve Stimulation
Before the case starts, we need to come up with our neuromonitoring plan, gather our supplies, and prepare our program.
The Plan
We will be mapping the hypoglossal nerve and monitoring train-of-four to document 4/4 muscle activity.
We’re going to be recording from 2 muscles, the genioglossus (activates during medial branch stimulation), and the hyoglossuss/styloglossuss (activates during lateral branch stimulation).
The Supplies
– 2 paired electrodes for EMG
– 2 paired electrodes for stimulation and recording of a TOF.
– 1 single electrode for a ground
– 1 monopolar or bipolar probe
– 1 single electrode for a reference if you chose to use the monopolar probe.
The Program
This one is going to be as easy as it gets. Chances are you already have a thyroidectomy protocol already created that you can use as a template and make some adjustments to it.
These responses are going to come in pretty quickly, so you’ll want to set your screen to display at 1-2 ms/Div and 500 microV/Div.
Options you might find useful are to keep the colors different and use a waterfall to help capture the images for documentation.
The Anesthesia
Compared to what we’re used to covering, these cases are fast. The pt is supine, so the setup is fast too. If anesthesia doesn’t need muscle relaxation, that would be best. If it’s part of the plan, make sure to cover your needs. No different than a thyroidectomy plan.
The Setup
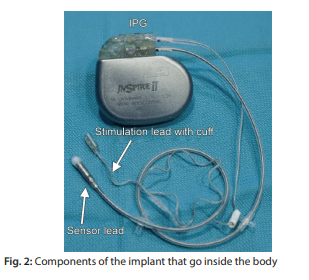
The genioglossus muscle is the one that sticks the tongue out and will help open the airways during sleep, so this is the muscle we are targeting. We want these electrodes stuck vertically into the floor of the mouth out lateral, avoiding the submandibular duct.
The hyoglossal and styloglossal muscles bring the tongue back, so we do not want to see responses on these. You’ll stick these by placing them in the lateral portion of the tongue under the mucosa.
During the Case
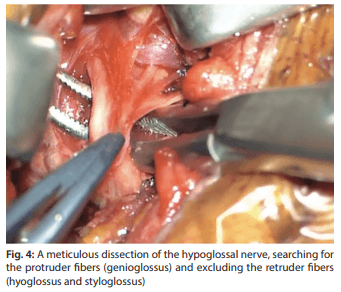
After the surgeon cuts the skin, he or she will dissect the hypoglossal nerve looking for the separation of the lateral and medial branches of the hypoglossal nerve. This is usually near the vasa nervorum.
This is our time to shine.
We make sure the patient is 4/4 for train-of-four and our stimulator (and return for monopolar probe) are sending out 0.1-0.5 mA of constant current. The pulse is monophasic rectangular with a width of 100 microsec. A rate of 33 Hz will work.
The information we’re looking to give the surgeon is:
– no response
– yes, response in the genioglossus
– yes, response in the hyoglossus
– yes, response in BOTH the genioglossus and the hyoglossus
The ideal electrode placement will be with a good response on the genioglossus with no response in the hyoglossus.
Monopolar vs Bipolar
With the close proximity of the medial and distal branches, as well as to where the surgeon is placing the electrode compared to the functional branching, we have to discuss our probe selection.
Our stimulation intensity is low, which lowers our concern with cross-talk of nerves from the spread of monopolar stimulation.
Also…
Our stimulation is low, and maybe that could lead to stimulation of some fibers and not others.
2 potential weaknesses to consider.
But when we consider the goal of the surgery, we might find the decision to be easier.
We are looking to assist the surgeon in placing the electrode that will only stimulate the medial branch and not the lateral branch. So we might err on the side of additional spread over lower penetration and rely on the morphology to help differentiate what we have.
That’s what Sturm, 2020 did.
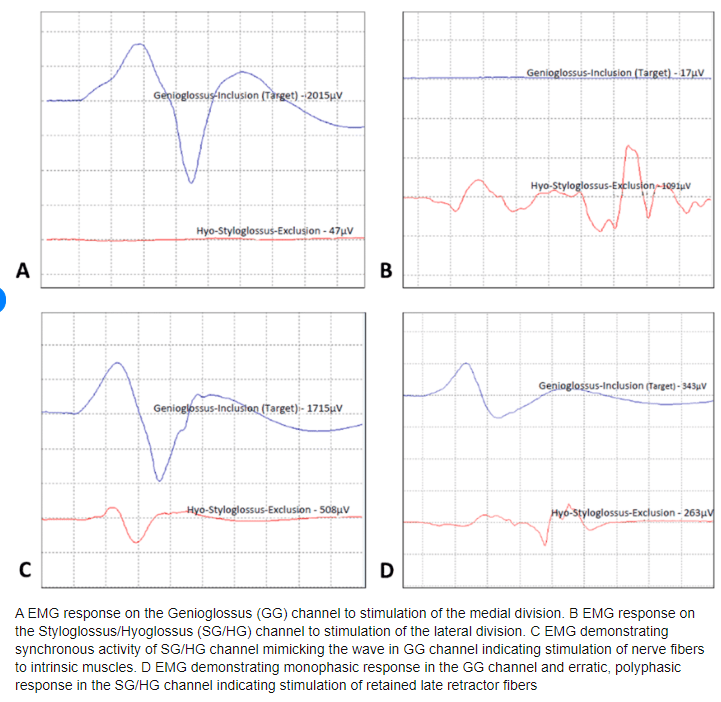
What they were able to conclude was the monopolar probe was able to pick up some additional mixed activation that the bipolar probe was not. After further dissection and repositioning of the stimulation cuff, the results were reduced mixed activation.
You can see in the image above “C” is more cross-talk and “D” is the unwanted mixed activation (more likely to cause some tongue retraction and reduce the desired effects.
One last note about tcMEP
There hasn’t been any permanent injury of the hypoglossal nerve I could find. There was an incidence of about 1% of transient weakness, most likely due to mild, focal demyelination.
That leaves us with a couple of questions:
– is that enough to justify using tcMEP?
– would we be able to isolate reliable corticobulbar motors?
– would tcMEPS be useful in preventing injury?
I’ll be keeping an eye out for any further discussion here.