Steps To Becoming A Surgical Neurophysiologist (Guest Post)
Joe’s Notes: I don’t really ever write it after my name anymore, but I am also an OTR (Registered Occupational Therapist). If I would have stopped there, I don’t think I would have learned about becoming a surgical neurophysiologist. There was absolutely no mention of it.
After finding out more about Tom’s background in physical therapy, and knowing all the different roles he’s had in neuromonitoring, I asked him to put a post together for those in the physical therapy or occupational therapy field considering getting into the neuromonitoring field.
If you would have asked me 3 years ago to make a prediction about what neuromonitoring would look like in 2016 (even with the G0453 Code), I would have said we will start to see an influx of more OT’s, PT’s and nurses.
I would have been wrong.
There’s probably a couple reasons for it:
- They are still in demand in their own fields.
- They can find some positions that are your typical 9-5pm.
- They’ve been hit by changes in healthcare, but probably not to the same extent as others. Chiropractors, audiologist and Ph.D.’s have found themselves in tough markets.
- While the average pay in IONM is probably higher, they may find value in other perks of their job vs IONM.
- They have large associations and more of a community presence. Throw a couple of rocks in any major city and you’ll wind up hitting a nurse in the head on your third try. That same city might have 20 surgical neurophysiologist total. It’s hard to leave your friends.
- The word just hasn’t made it to those folks. There is an opportunity for them, and they have a very good chance of doing well with neuromonitoring as a career.
But the fact that physical therapist and occupational therapist have a great understanding of the human body, have been introduced to surgeries that they do the rehab on and have been at least introduced to neurodiagnostic studies like nerve conduction studies and electromyography, they have a pretty solid foundation. Most companies are looking for that caliber of recruit.
Considering that this is still a growing field with new opportunities, we still might see some more PT’s, OT’s and nurses. If the oversight rules change again and allows non-physician doctors to perform oversight, I’ll probably reclaim that origional prediction. There are a lot more doctors in those fields than there used to be.
On with the post…
Thomas McGee, CNIM Answers The Question – How Did You Start In Physical Therapy And End Up Monitoring During Surgery?
I am a Surgical Neurophysiologist, an IOM Tech, a glorified electrician, the guy in the corner, I even have the nickname “Twitches”, all names for the same position – I’m a guy who ‘monitors brain waves’ for a living…
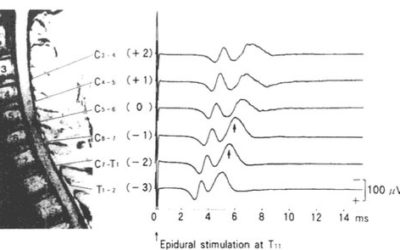
First, a little bit about Intraoperative Monitoring (IOM): Surgical neurophysiology is an exciting, ‘new’ field – one that has its roots starting from Dr. Wilder Penfield’s description of using EEG in the Operating Room (OR) in 1939 for determining the location of a seizure focus, to first describing cortical stimulation experiments which were first published in 1951, to the use of somatosensory evoked potentials being used intraoperatively in the 1970’s (on one and two channel machines!), to adding more refined and elaborate techniques in that same OR environment. Much study has gone into refining these techniques, and we have numerous people to thank for their pioneering studies and advances in the field.
Now, a bit about me. I am a Surgical Neurophysiologist with Sentient Medical Systems and started August 4, 2003. I also am a Director of Training for the company as well. My career has been filled with a variety of positions, including Clinical Manager (now called a Regional Director), and Regional Director (which is now called a Vice President of Operations). I left a career in Physical Therapy to learn how to do monitoring, and the rewards have been more than I ever expected.
The PT background that I had I wouldn’t trade for anything. My Physical Therapy education was filled with anatomy, physiology, kinesiology, neuroanatomy, and well as orthopedic surgeries. It is great training to apply monitoring techniques in the OR.
In the first few surgeries that I attended, and I believe this experience is true for most, that the trainee is wide-eyed trying to take everything in – the noisy environment, the quick pace of everyone, the concept of seeing a person have surgery – it’s surreal. It’s a good idea to have an idea of what to expect before going into the operating room. YouTube wasn’t around when I started, but it’s such a great help today! If you are going to see a surgery, or even if surgery interests you, there are videos of just about any given orthopedic surgery (don’t do this at home!) I remember the first time that I saw a surgeon take a Rongeur and remove a spinous process from a lumbar vertebra! Shocking! You soon get used to this. The OR environment is not for the faint of heart. A quick side note: There is no ‘simple surgery’. I’ve seen procedures that are seemingly simple have complications for patients, and very complex surgeries go well for patients.
The title of this article is how I became a Surgical Neurophysiologist. Back in those PT days, I was looking at alternative careers. 14 years in that profession took its toll on me. I took some computer programming classes at night to build my technical background while doing PT during the day. I took a 9-month foray into the world of computer programming and found that the environment I was in was not a healthy environment for me. So I went back full time into Physical Therapy. One of the therapists that I worked with was (and still is) married to a Neurologist who was the Medical Director for Sentient at the time. The PT called me and said, I know you’re looking to get out of Physical Therapy, and you should look into this new field. It combines several of the strengths that I have: the technical background, the patient care aspect, and also can be highly involved in surgeries. Wow, did that sound exciting! So, I contacted the Sentient manager who lived in the same area I was living and started talking with him about this new field. Thanks, Amy and Don!
Over the course of a couple of months, he and I talked and talked. I don’t know about you, but at some point, there’s enough talking – I am a visual learner. So I asked him if I could shadow him on a case, and after the appropriate approvals were gained, we waited for the right day. Fourth of July 2003, he called me up and said that there’s an emergent surgery where someone had fallen and broken their vertebral column. Monitoring was requested for that surgery to ensure the integrity of the spinal cord. I talked it over with my wife, we agreed that this was a good idea, and I went in to see the surgery. I was hooked!
Talk about eye-opening! The fast pace of the procedure, the interactions with the surgeon and anesthesiologist, the interview with the patient prior to the procedure, the computer data collection, seeing the instrumentation placed, – the whole deal – was quite intriguing! If you do the math, you see that I started with Sentient a month later! I haven’t looked back wondering about those PT days – this is the career for me! Thanks John for showing me the way!
One more thing, in case you are wondering, what does the ‘normal’ schedule for a Surgical Neurophysiologist look like? In my PT days, the days were 7-4, or 8-5; regular everyday schedules, all days were the same. In IOM, schedules are different. The differences are due to a number of different factors, such as the monitoring volume of the area or facility in which you work, the case complexity, skill of the surgeon, other co-workers in your area, etc.
Let’s look at these factors:
- Some areas are not as busy as other areas. There are reports of some people working three days in a given week. Others are working all 5 days and also have overtime, or work the weekends. There are trends in surgeries that show up on a cyclical basis, such as scoliosis season, a time just at the end of the school year (usually starting in May or early June), and allows the children to recover from their surgeries over the summer.
- Case complexity: It’s not a surprise to think that certain surgeries take longer than others due to the amount of surgical intervention required. A one-level anterior cervical discectomy and fusion on average will be shorter than a 5 level anterior/posterior cervical fusion.
- The skill of the surgeon: I’ve been involved in one level anterior cervical fusion surgeries that have been completed in 45 minutes, or the same surgery with a different surgeon taking 8 hours. It’s more than just a surgeon being unsure. If a patient has had a previous surgery, there’s additional scar tissue that must be navigated safely to avoid injuring other structures, such as major blood vessels.
- Other co-workers in your area: If you’re the only Surgical Neurophysiologist in your area, then you’re going to be involved in every surgery. If you have others sharing the load, then you won’t be quite as busy. There are definite business decisions that are to be addressed – ultimately, in just about every scenario, the role of having to monitor means that the company has to be at a minimum covering costs and hopefully making a profit.
Let me tell you, just in case you don’t have a Physical Therapy background (and a Physical Therapy background is NOT necessary), if this sounds like something that intrigues you, feel free to contact me, Joe, or any of the Surgical Neurophysiologists out there to find out more about the career opportunities that exist.
The path to get into this field is varied. At the time of this writing, there is really only one bachelor’s degree program that is geared toward including Intraoperative Monitoring. The few graduates that I’ve seen come through that program at the University of Michigan have really shined! The second and most utilized pathway that people come into the field is by having a bachelor’s degree, preferably in neuroscience, or higher degree (Master’s or Doctorate). I find that Chiropractors and Audiologists are huge in the field, but in the time that I’ve managed this territory for Sentient, I’ve had an MD, RN, DC, Audiologist, EEG Tech, Paramedic, and even a hardware representative work with me, among others. The third pathway that folks come to the field is through having another neurodiagnostic credential, such as an R. EEG. T, or R. EP. T. More information can be found on those certifications at here or here.

Thomas McGee, CNIM
Director of Training in Surgical Neurophysiology
Tom has transitioned from Regional Director and upper management to his current role of Director of Training and Education. He now oversees the management of Sentient Medical’s Clinical Trainers, as well leads classroom lectures for Sentient’s Fellowship program and creation (and on-going tinkering) of their CNIM coursework.
In-House Or Contractual Neuromonitoring Company: Where To Work?
IOM Jobs: In-House Or With A Contractual Neuromonitoring Company: Pros And Cons With the amount of people looking to get into neuromonitoring, and some of the larger companies slowing down their hiring till the dust settles on these billing issues, it seems like most...
Neuromonitoring Job: Preparing For The Interview
Interviewing For A Neuromonitoring Job If you got the call for an interview for a neuromonitoring job, then you've already wowed them with your killer IONM résumé. Now comes the part that everyone love... selling yourself without sounding like a braggart, and then...
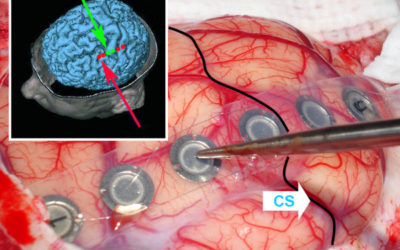
Direct Motor Evoked Potentials Using Surface Electrodes: Pros and Cons
Direct Motor Evoked Potentials Continuing on from the post about intraoperative monitoring for gliomas (and trying my best not to ramble on too much in this post), I'd like to discuss some pros and cons to using a surface electrode strip as an anode directly on the...
7 Reasons To Love Sugammadex For Neurophysiological Monitoring
Neurophysiologic Intraoperative Monitoring With Sugammadex Let me start off by saying this... I have no experience with the use of Sugammadex during neurophysiological monitoring. The drug was denied FDA clearance in the USA in 2008, so maybe some UK readers can chime...
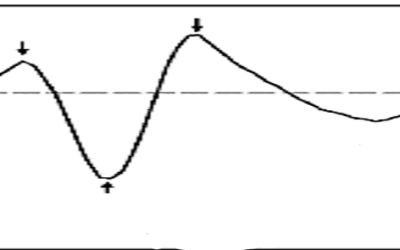
Variability In Somatosensory Evoked Potential Test: Summing It Up
Somatosensory Evoked Potential Test Variability In my previous 2 post about temporal dispersion and somatosensory evoked potential test variability, I went over how to ID trial-to-trial variability, how to handle it and what was happening to the waveform. I'm going to...
Follow Up Post: SSEP Increased Variability vs. Increased Latency
SSEP Increased Variability vs. Increased Latency: A question from a reader... In my last post, I talked about using the waterfall function to better determine your SSEP baselines, as well as how using it can be helpful in determining your level of confidence with the...



Thomas, thanks for your well written article. As a Physical Therapist (PT) who has found a home in surgical neurophysiology, I am pleased to see other PT’s in the IONM field. Surgical Neurophysiology is a natural extension of the clinical evoked potentials done by PT’s specializing in clinical electrophysiology. Early on PT’s made significant impacts in the field of IONM, only to find politics were not on their side. Over the last few years it seems that everyone has learned to play in the same sandbox and PT’s are returning to the OR.
I am a big advocate of PT’s entering the field as well as PhD’s, OT’s, audiologists, chiropractors, and other medical providers. Each provider type brings the strengths of their own specialty with them to add to the field of IONM. This diversity has given the IONM knowledge library a great depth and breadth of information. We may complain that the lack of standardization has hurt the field when it comes to licensure and reimbursement but the upside is that we gained a diversity of thought that will provided better care for years to come.