Signal Improvements In tcMEP and SSEP During Spine Surgery
What does everyone want for IONM?
Needless recording electrodes and cordless monitoring equipment. Both would be great — if it actually worked like the alternative.
But I can’t be alone in thinking this: telling the surgeon I’ve had improved signals as a result of some surgical intervention is the single thing I want most for IONM. And it’s been that way since I started in 2007.
It’s great in Chiari repairs using ABRs and MVD of CN 7 for hemifacial spasm — and I want it for all spine cases.
It would open up so many doors for IONM’s use cases, especially coming on the heels of the current “experimental” questioning through non-scientific, incentive-based claims of Cigna.
But it’s always been a case of wishful thinking.
And when I’ve worked with surgeons expecting it because “the other company told me signals got better every case,” I can’t help but cringe.
Because I know — as many of the experienced clinicians with validate — it just doesn’t work out that way.
Sure, I’ve had cases where major changes of improvement occurred. But not as many as you would think from someone spending years working at a level 1 trauma center. It happens so few times, it’s best to look for other explanations first (change in BP, change in anesthesia, etc.).
And then came a curveball; a glimmer of light. An actual research paper from 2020 titled:
Clinical Significance of Improved Intraoperative Neurophysiological Monitoring Signal during Spine Surgery: A Retrospective Study of a Single- Institution Prospective Cohort.
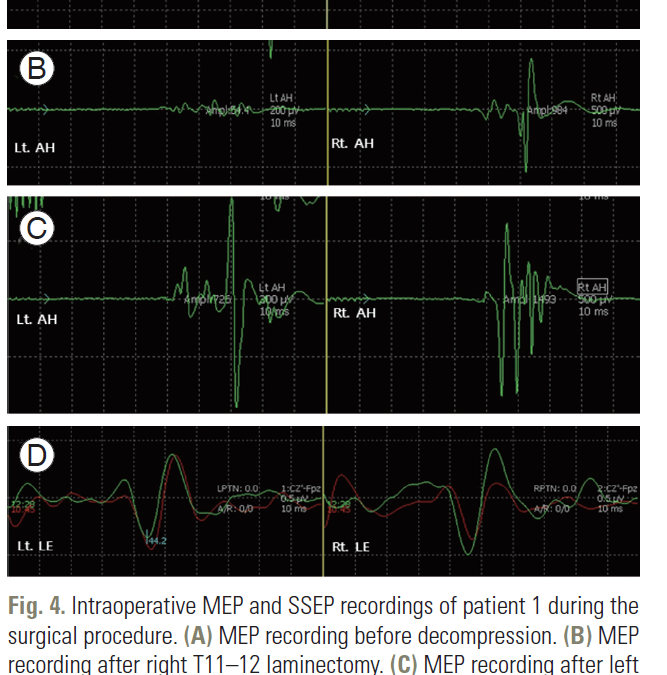
In this paper, the authors are looking for changes in SSEP and tcMEP during spine surgery, as defined as:
“A significant MEP improvement was defined as a greater than 100% increase in amplitude or the appearance of a distinguishable waveform during surgery, and improvement in SSEP was defined as a greater than
100% increase in amplitude or decrease in latency of at least 6%.”
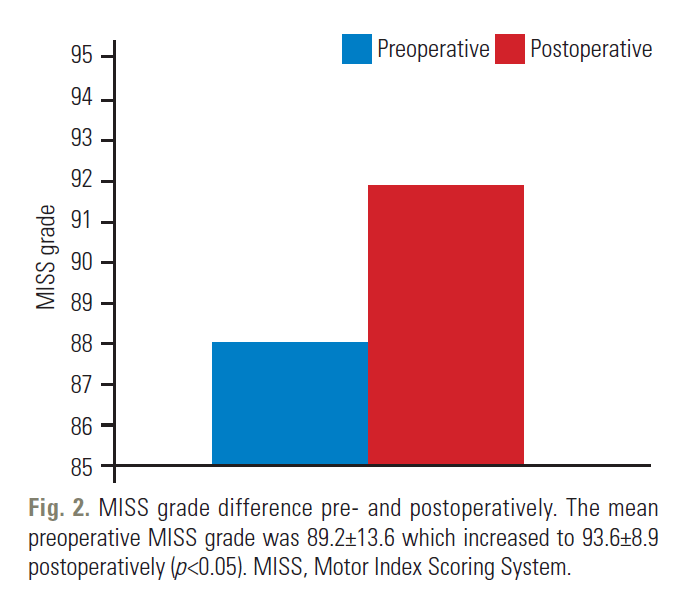
29 of the 317 patients (9.1%) over a 4 year period met this criterion. The Motor Index Scoring System and self-reporting questionnaires were used as the measurement tools.
And just check out these results. It really pops out and catches your eye when reading the report.
Time To Revamp The Way We Practice IONM and Communicate With Surgeons?
Perfect. This is the study I’ve been waiting for over a decade to get published. Being able to track patients after the surgery could be the thing that unlocks it all, right? After being a decade-long naysayer, I’d gladly eat crow and admit I was wrong.
I mean, what do you do when you’re presented with new evidence?
But like all good Bayesians looking to update their priors, I need to mind my emotions and not let them drag me out of reality as we understand it into reality as I’d like to be true.
Because I really, really want it to be true and go all-in on it.
As a solid rule of thumb, when you end up seeing the information confirmation you wanted, it’s best to jump to the other side and see if you can disprove it.
A View From the Other Side of the Table
So let’s look at some of the weaknesses of the study first.
As mentioned by the authors, this was a really small sample size, spanning different surgery types, included in a retrospective design. Even when taken in addition to other articles published (Bouchard et al and Visser et al), we barely have something to hang our hat. It’s not a nothing-burger, but rather a single data point.
So we should update our priors appropriately weighted and in concert with the evidence presented in the context of our past understanding.
When we find ourselves in this situation, it is prudent to not go all in or all out. Not “you see, here’s the proof,” but rather “let’s see what, if anything, we can take away from this to build upon.”
In our world of headlines and fake narratives, this is a critical skill set to develop — and continuously remind yourself. It’s an uphill battle worth the fight.
A Skeptic, Not a Cynic
Knowing I would love to tell a surgeon something along the lines of “you have a X% increase in MEPs verifying the cord is now decompressed and that is predictive of a full motor recovery within 30 days,” but couldn’t, I’ve become guarded against any competitors saying something similar.
Programmed, even, through incentives and repetition.
And when those claims are made to me, I’ve shut it down before even assessing the evidence. Because that’s the narrative I’ve told myself about myself and the company I choose to work for: evidence-based and on the up-and-up.
While bought-in it isn’t a bad place to be, it does have faults. Extreme takes like this lead to acting cynical, or coming from a place of disbelief, instead of being skeptical, or coming from a place of questioning. A subtle, yet important, starting place.
So when I read a paper like this, where the authors conclude “… we urge surgeons to consider the
improved IONM signals as a sign of successful decompression,” I, admittedly, took the bait and prepared myself for a flip flop.
How To Social Media: Step 1 – Read the Headline. Step 2 – Confirm Your Priors. Step 3 – Share. Step 4 – Indoctrinate.
I saw this article come across in a LinkedIn post and I immediately forgot about all my clinical experience and discussions with others in the field, ready to bow down to the authority of a published article. After being adamantly opposed to the possibility, I swung too far as being too ready to accept it (at least for a brief moment).
This is where I fell flat and hope to do better next time: from cynical to fanatical in a single headline, all the while a proper dose of skepticism reigns superior.
Now, this paper should be part of our understanding — a data point to reference under an appropriate weight — but plays a different role than answering the question we want it to: can IONM be used in spinal cases to determine the level of decompression of the spine/nerves as a predictor of outcomes?
Instead, it gives evidence that directing our collective energy and curiosity could be a fruitful endeavor. Creating more questions than answers, one might start to wonder about specific items to support the claims.
- What surgical procedures does this lend itself to?
- Which modality is a more sensitive tool to use?
- Which patient population would this work best/worst in?
- What other variables need to be controlled?
- Does the timing of an injury matter?
- Does the severity of an injury matter?
- Does this work on both central and peripheral decompressions?
- Do we reset the baselines after improvement, or should we expect a wider bandwidth/variability of signals?
- Is there a time frame requirement as to when we see improvements?
- Does this point to a specific surgical procedure as more optimal for productive decompression?
- What research design is optimal?
- Is the chosen alarm criteria optimal?
- Are the chosen post-op measurements optimal?
- Does 0% improvement speak more to the patient’s pathology or the surgeon’s performance, both, or neither?
- How does this affect the total cost of care?
- Does this make IONM more useful in surgeries insurance companies are looking to decline payment?
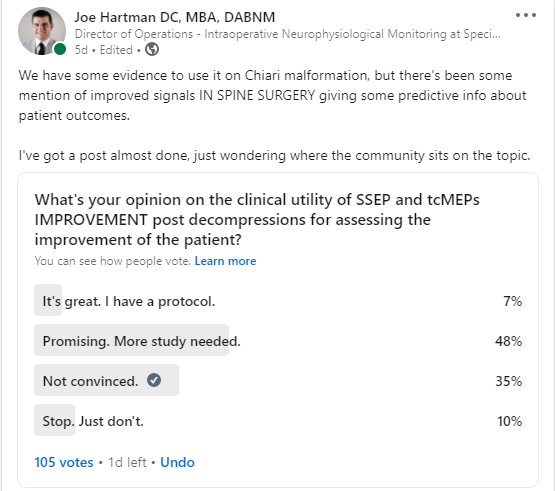
I’m sure there’s plenty of other important questions to answer. Looks some of you are already coming up with more questions and looking for answers.
So, You’re Saying There’s a Chance…
If you’ve read more than a handful of research papers, one conclusion you can easily draw is there is never one conclusion to draw. Chalk some of that up to suboptimal science (making claims, instead of raising questions, with small sample sizes, poorly controlled studies, incorrect conclusions made by the authors, etc.). But we also expect refined protocols and new, promising techniques to continue the way we practice our craft. This is all part of science’s slow march towards the truth and allows for evidence-based medicine and recommended best practices.
During that slow march, what you end up with is multiple recommendations (For example, motor evoked potential alarm criteria: all-or-none, 50% drop, a decrease in the duration and complexity of the CMAP, changes in the threshold levels, a mixed bag — just to name a few) until things finally start to shake out. We might find ourselves in a perpetual gray area instead of a cut-and-dry, updated version of “do this, not that until something better is proven.”
We are not, however, without a path to follow. Straying out of bounds due to either not staying up to date (excusing ignorance) or purposely practicing outside of acceptable standards not only poses a problem to patient safety, but also the overall validity of neuromonitoring.
Naturally, that poses a problem to our collective IONM tribe. Our ability to coordinate is one of mankind’s greatest traits, so we are hardwired to act harshly against those disrupting that which glues our social norms together — trust.
Trust, you might have heard, is earned over time. And easily destroyed. Our problem isn’t just people losing trust because the service we provide didn’t live up to its billing. It’s that our environment acts against the evolution of trust. That may be marginalizing our ability to own our actions — that we’re “merely” products of our environment. But as game theory reminds us, we are each others’ environment. In the short run, the game defines the players. In the long run, it’s us players who define the game
But That’s Not Fair!
Hearing competitors using improved SSEPs or tcMEPs for spinal decompression as a part of the service provided vs what I/we are willing to produce puts me/us in a precarious position. A surgeon could see it, unfairly, as a differentiator.
This is the balance of social coordination of the collective group with the competitive interplay of companies/clinicians. Neither Machiavellian nor Draconian rules apply. This is a matter of “playing fair.” And there’s an unspoken social contract in place. It always will be, too.
Are You Hunting Stags or Hares?
In the context of this social game — an assurance coordinated game — we can understand what the players do. In coordinated games, you tend to go further if you go together (we all do what’s best practice), rather than alone. If you do choose to defect (you are telling the surgeon they’ve got improved signals on your cases without knowing if it means anything), you’ll only win if no one else knows any better.
So if we were looking to maximize IONM’s overall utilization, we’d want to go at it together. And this might become more clear in the context of a game, the one where we’re all hunting for more cases.
What you’d want to do if you’re hunting the big game, like a stag, is to hunt in a coordinate pack following the unspoken social contract powered by trust. It’s harder but worth it. Alternatively, you can decide to not work with the group’s interest to maximize everyone’s gains by shrinking the pie and trying to take more. This is turning your back to the group hunting the big game and take the easier path of hunting hares solo.
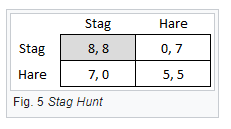
Using the box above as our payout tool, all of us are hunters choosing how to hunt (sell our services). It’s harder to hunt a large stag (stay honest in our promises), but the payout for everyone is larger when we do together (8,8). The worst spot to be in, of course, is stag hunting by yourself (other people are lying and selling more, where you get 0 and they get 7). If someone defects (embellishes the truth for a faulty differentiator, or hunts hares) they earn less if alone (7, 0) and even less if everyone is doing it (5, 5). This is because someone will call them out on their lies and the overall pie shrinks.
Let’s not shoot ourselves in the foot. We shouldn’t defect when it makes sense to hunt stags and eat more. This doesn’t mean to curtail curiosity or stop progress. Boundaries were meant to be stress tested. It also doesn’t mean competition is dead. Work to be better every day.
At the same time, do not ignore Chesterton’s fence with our exuberance and understand the reason for the constraints already in place. If there is a constraint in place, ask why it is there first.
We should look to maximize our gains by expanding the pie over trying to get more slices of a smaller one. This is a coordinated movement of thousands of people involved, well outside of Dunbar’s number. While this is easier said than done, such a coordinated move leads to what should be (IMO) IONM’s collective north star: Legitimacy.
Legitimacy: A New Perspective of What I Want Most For IONM
After reading this paper, and piecemealing together a couple of adjacent thoughts, I’ve changed my mind on what I want most for IONM.
Looking at improvements of signals in spine surgery is too focused. I’d be wishing for a million dollars instead of the money tree, missing the bigger prize.
There’s a larger overarching theme I see as mission-critical for IONM. It is the pursuit of legitimacy.
And while we all have a firm grasp as to the definition — and may make the argument legitimacy has been established — maintaining it as the end target should remain the end target for all coordinated games that exist. This isn’t something we can achieve and then pour on concrete to solidify. Legitimacy is fluid and lives on a spectrum.
Hunting hares (for example, defecting against the established norm that improvement in SSEP and tcMEPs during spinal procedures is not a well-established marker to give surgeons any predictive information) goes against the established culture of accepted norms, beliefs, practices, and procedures accepted. It frays trust, or the glue holding it together. A loss of trust erodes the legitimacy of that thing and shrinks the pie.
With this in mind, we can explore common theories of legitimacy and use the mechanisms at our disposal to create powerful social coordination expanding beyond Dunbar’s number. While not an exhaustive list, here are some considerations when targeting legitimacy at any level.
Brute force
If you look at the second link in this post, you can see two heavy hitters going at it through brute force. Cigna looking to deny claims and Dr. Mino speaking “On behalf of over 34,000 orthopaedic surgeons and residents represented by the American Academy of Orthopaedic Surgeons (AAOS)” using the power of authority in the defense of IONM’s legitimacy.
Drawing on one’s authority currency, which is a finite resource, can propel narratives forward into acceptance. While we must be careful of falling prey to authority bias, it’s easy to see the benefits of using brute force (responsibly).
So as we elect our own governing boards, we need to keep each candidate’s ability to carry forward IONM’s legitimacy top of mind. In an ideal world, it would be one of our own with the authority to properly disputes these claims, backed by legitimacy.
As we look to find our own way in this space, carving out your own opportunities in the direction of legitimacy is like swimming with the current.
Continuity
Something becomes established and proceeds over time. Often referred to as the Lindy effect, where you have higher confidence in something that remains prominent over time (like Shakespeare’s writings or EEGs on carotids). If there was established legitimacy at time T, then legitimacy if preserved at time T + 1.
Fairness
As social creatures, we’ve evolved BS detectors. These help the group sniff out someone looking to place themselves above the rest, which we would call unfair. Succeeding on a level playing field — because elevation does matter — helps confirm legitimacy. As such, acts of money grabs (see billing practices > $100K) does little to help our position as a legitimate service with justifiable cost, while placing CNIM credentialed clinicians in the surgical cases is par for the course.
Process
How a conclusion was reached brings legitimacy to the narrative created. Was it done through thoughtful and thorough science, or was it a slick YouTube video? Did you come to your conclusion with enough skepticism, or did something confirm your beliefs… enough.
How you got from A to B is as important part of the story as reaching B.
Performance
Are the outputs satisfactory to the inputs given? Is our monitoring providing value that can be relied upon to prevent injury at the cost to the hospital/patient? Creating claims of performance we cannot satisfy poses a threat to our legitimacy.
Participation
This is where proper education comes in. People are prone to continue on with a decision they were a part of making. We yearn to be consistent with our previous actions. Change is pain.
So we want to get it right and be seen as a good decision-maker.
For example, allowing hospitals and surgeons to make informed decisions on choosing the best provider allows them to participate in the outcome they are seeking, adding to the legitimacy of the group selected.
Legitimacy Leads To Exponential Growth
Using these points is how IONM legitimacy, or a pattern of higher-order acceptance, continues on.
But not linearly.
Because as legitimacy increases, it moves the actors from not only acceptance but influences actions/efforts to reinforce the outcomes (as they expect everyone else to do the same). This creates a network effect as each node adds value to all other nodes, creating more value to new participants accepting of it, who reinforce the outcomes, to produce more value for new entrants, and on and on.
From there, we better solidify the things we want to hear, like “standard of care” and “valued members of the surgical team.” Legitimacy ensures that thing as the base reference to which everything is judged against.
Summing Things Up
Am I ready to pop the cork and celebrate?
Not quite yet. I am happy to see research being done in this direction. There’s seems to be potential here, but probably more misinformation and assumptions than that. It is reassuring to see others avoiding the cynicism, staying skeptical, and looking for answers to questions commonly asked.
But I still seem to be a little more skeptical than others, even after my moment of euphoria.
But progress will be our guide to accurate predictions in positive recovery post-decompression (should that be in the cards). And progress is the fruit of the scientific method, which is, again, a form of a coordination game in the direction of legitimacy.
The thing I really want most.