Intraoperative Bulbocavernosus Reflex
Surgeon: Isn’t there anything else you can do to monitor the sacral nerve roots? That’s the area I’m most concerned about today…
Me: Well, there’s the intraoperative bulbocavernosus reflex. That would monitor the pudendal nerve up through the sacral roots.
Surgeon: That sounds good. Why haven’t we done that in the past?
Me: Because the clitoral and dorsal penile nerves are small sensory nerves, difficult to stimulate and are difficult to reliably obtain in the operating room, they are seldom used. More importantly, we need to consider that these nerves are subserved by multiple sacral roots, and injury to one root may not produce a significant change in the response.
Surgeon: Penile nerve? So you stimulate off his penis? Forget it. That sounds horrible.
And that’s how the one conversation went with a surgeon when talking about the intraoperative bulbocavernosus response. The part where I told him that it might not be the best test for sacral root monitoring was a deterrent from using it, but stimulating off the kid’s penis was the nail in the coffin.
So the rest of this post comes from no experience using it in the operating room on my part. But studying for my DABNM exams, I did put together some notes on the subject. In an up-and-coming article, I will post a Propep article demonstrating the need for monitoring the pudendal nerve during robotic prostatectomies, intraoperative bulbocavernosus reflex needs to be revisited.
But in these prostatectomy surgeries, we aren’t talking about monitoring the sacral roots, but rather the peripheral pudendal nerve itself. That’s a totally different ballgame.
And since my one conversation with that surgeon about intraoperative bulbocavernosus reflexes during a tethered cord surgery, I’ve learned a couple other tricks to better optimize responses.
We’ll get into those IONM optimization tips, but I feel that I should go over the BCR response and setup for intraoperative neuromonitoring first.
Intraoperative Bulbocavernosus Reflex: The Response
The BCR is a polysynaptic reflex in which stimulation of the glans penis (clitoris) results in contraction of the external anal sphincter.
So stimulation over a sensory nerve travels orthodromic to the spinal cord, synapses happen, and a signal is sent orthodromic out to the external anal sphincter for a motor response.
Sounds a lot like an H-reflex, doesn’t it? The H-reflex is similar to hitting a tendon with a reflex hammer and getting a muscle contraction at the same muscle. The difference is the H-reflex uses electric current to stimulate the nerve axons, whereas the reflex hammer causes mechanical fast stretch on the muscle spindles. So the H-reflex is a little more simple by bypassing the receptors needed to grade the response. But both are monosynaptic (maybe).
That’s not the same with the bulbocavernosus reflex. In order to elicit this response during a physical examination, the doctor will either pull on an already placed catheter or squeeze the glans penis or clitoris and monitor for contraction of the external anal sphincter. This test is done to help assess patients during spinal shock. Intraoperative bulbocavernosus response uses electric current and again bypasses the receptor activation. The difference from the H-reflex is that this is an oligosynaptic response, or has a couple additional synapses in the arc (so more than monosynaptic, more than disynaptic, less than polysynaptic).
Although the monosynaptic H-reflex depends on the excitation of muscle afferents while cutaneous afferents mediate the oligosynaptic BCR, fundamentally similar mechanisms of facilitation (and inhibition) of alpha motor neuron pools at the S1 and S2–4 levels respectively may be presumed.
An additional reason to consider them similar mechanisms is that they might actually be more similar mechanisms than what is often depicted. According to (Burke, 1984), the H-reflex might have both monosynaptic and oligosynaptic contributions, not just the monosynaptic arc we see in most textbooks.
This is important for us to realize when looking at intraoperative bulbocavernosus reflexes, and H-reflex for that matter. I think most of us are aware of the reliability of any evoked response under anesthesia as the number of synapses increases.
But we also need to appreciate the fact that there could be inhibitory interneurons activated by low threshold motor neurons that may prevent the excitation of higher-threshold motor neurons.
Intraoperative Bulbocavernous Response: Collecting Data
This is where I lost the surgeon. There are certain anatomical areas where needle placement makes most people cringe. Recording from the lateral rectus is one. Stimulating over the penis or clitoris is another. The cathode is placed proximal to the anode. Recording electrodes are placed in the external anal sphincter.
Pro Tip #1: This is a very small response that is difficult to collect. Unlike the picture above, you may consider using a referential setup to improve the sensitivity of data collection. (Rodi, 2001) showed that the median amplitude was twice as large using a referential over bipolar recording setup.
Pro Tip #2: The external anal sphincter is a very shallow muscle. If you’re just jabbing it in there, you’re probably going too deep. Verify placement by stimulating and watching for contraction.
Place each recording electrode through the skin approximately 1 cm lateral to the anal orifice, parallel to the direction of the anal canal.
Testing of the recording electrodes can be conducted by visual inspection of a muscle twitch after stimulating at 10mA, train of 4, ISI of 2 ms. Once confirmed, then place the electrode in the appropriate pod.
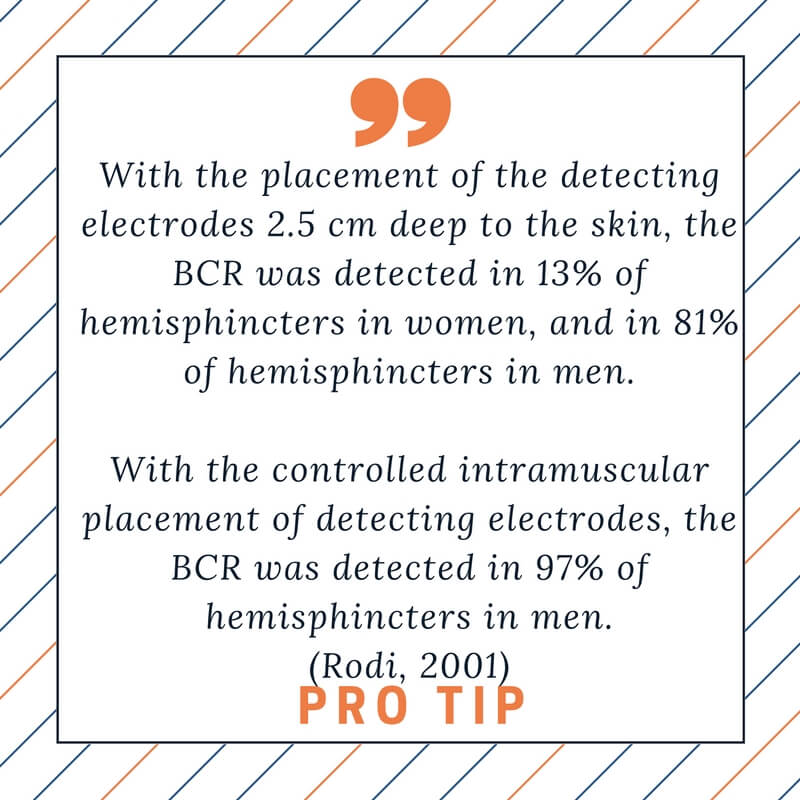
Pro Tip #3: Most of the early studies used a single stimulus to elicit an intraoperative bulbocavernosus reflex. Later studies, like (Rodi, 2001) suggest using multiple trains. Their numbers reflect the importance of using multi-pulsed stimulation. The acquisition rates were the following:
- Single pulse – 50%
- Train of 2 – 75%
- Train of 3 – 95%
- Train of 4 – 100%
- Train of 5 – 100%
Likewise, (Skinner, 2007) showed that using a double train increased the number of turns and improved amplitude size by 30% or greater in 79% of subjects. They were using the following stimulation parameters:
Train Stim = 333 Hz
Train Count = 4
Pulse Duration = 500 μs
Stim Current = 2 –50 mA
Double Train
ITI = 75–250 ms (more study needed)
Intraoperative BCR: Some Downside
Like all modalities we use in the operating room, there are some weaknesses that we need to be aware of. This list hits some of the most concerning ones:
- Difficult to collect overall, even more so in women. 20% of health, non-anesthetised women will not have a BCR.
- Multiple synapses along the pathway make it vulnerable to anesthesia. TIVA is and multi-pulsed stimulation is your best bet.
- There isn’t a lot of research out there to show how useful it is in preventing injury.
- There are no established alarm criteria. Skinner suggested a 90% decrease to be significant. That may, or may not, be appropriate when applying the modality to different surgical cases. To be useful, there might need to be different alarm criteria where the sacral roots are involved vs the pudendal nerve.
- Doesn’t do well to differentiate peripheral vs central, or motor vs sensory lesions.
- Difficulty in placing recording electrodes appropriately. Use the stimulation technique first to improve your odds.
I bet there are a couple old dogs out there that have used intraoperative bulbocavernosus reflex testing at some point early on in their career. Maybe someone is already using it on these robotic prostatectomies? I’d like to hear from some in the operating room experience.

Joe Hartman
Non-Compete Clause In IONM: Interview With An Attorney
Non-Compete Clauses In Intraoperative Neuromonitoring (Joe’s notes: In today's GUEST POST I interview Greg Barthelette, a lawyer in Boca Raton, Florida. Greg practices in a few different areas, most important to us is business law. I've used his services every time...
How Carpal Tunnel Syndrome Has Central Consequences That Affects Neuromonitoring
Carpal Tunnel Considerations In Neuromonitoring In the neurodiagnostic world, evaluating carpal tunnel syndrome is one of their bread-and-butter studies. For surgical neurophysiologist who works in the operating room, the topic of median nerve compression at the wrist...
IONM Manager: 7 Ways To Get Into Neuromonitoring Management
IONM Manager: 7 Ways To Get A Neuromonitoring Management Position There are far fewer neuromonitoring management positions available than there are clinicians that want them. If you’re working for a smaller contract company or in-house neuromonitoring group, you’ll...
Propep Surgical Introduces Monitoring During Radical Robotic Prostatecomies
Propep Surgical: Pudendal Nerve Neuromonitoring During Prostatectomy (Notes from Joe: Neuromonitoring used during prostatectomies has always made sense to me, so things made sense when Jann Rasmussen from Propep surgical talked to me about his new business venture....
SSEP Improvement Driving Surgical Decision Making In Spinal Decompression Surgery?
Is SSEP Improvement Sensitive For Detecting Complete Decompression Of The Spinal Cord Or Nerve Root? In an article that I wrote years ago, titled Brainstem Auditory Evoked Potential Used To Predict The Need For Duraplasty In Chiari Malformation Type I Decompression, I...
How I became a Surgical Neurophysiologist (From The Physical Therapy World)
Steps To Becoming A Surgical Neurophysiologist (Guest Post) Joe’s Notes: I don’t really ever write it after my name anymore, but I am also an OTR (Registered Occupational Therapist). If I would have stopped there, I don't think I would have learned about becoming a...