Triggered EMG for Total Thyroidectomy
In one of my previous post, I wrote about monitoring the recurrent laryngeal nerve with triggered EMG and the possibility of giving the surgeon misinformation. That misinformation (in that hypothetical scenario) could lead the surgeon down the path of making yet another mistake. The outcome was determined to be an unnecessary disaster.
The whole scenario that I concocted was based around the commonly used opinion that if you are doing a total thyroidectomy, and lose triggered EMG signals on the first side of the removal, then you should not proceed to take out the other lobe at that time. Rather, you should stop and assess the patient for post op deficits and recovery.
From what I’ve observed, as well as what I’ve learned from other’s experiences, that seems to be a pretty good policy. Remember… first, do no harm.
I had plans to return to the topic of triggered EMGs, especially used for identifying the recurrent laryngeal nerve, at a later time. But this morning I was reading a 2013 paper out of the British Journal of Surgery titled,
“Prospective study on loss of signal on the first side during neuromonitoring of the recurrent laryngeal nerve in total thyroidectomy”.
In this study, Sitges-Serra A, et al. challenge the notion that a signal loss in tEMG means that you should stage the surgery, so that the patient can be assessed for extent of the damage.
They go on to say…
After loss of signal of the recurrent laryngeal nerve dissected initially, there was a 90 per cent chance of intraoperative signal recovery. In this setting, judicious bilateral thyroidectomy can be performed without risk of bilateral recurrent nerve paresis.
Wow. That’s not the game plan we take with the surgeons at all. If we have a loss of signal, we take that as a sign that something’s wrong.
Here’s a few things that need to be observed about the study performed:
- There were about 300 patients included, and 16 had signal loss, or about 5.5% of their population base. That is much, much higher than what I’ve observed personally. My first hunch is to suspect technical error (machine malfunction, poor contact of the probe on the nerve, shunting of the current, anesthetic changes, etc.) It’s still possible, though.
- Even though 300 people is an OK sample size, 16 is not. There needs to be more people included with the group that is actually being studied for them to make those claims. The only claim that they can make with this study is that 5.5% of the patients having a thyroidectomy will have a neuromonitoring change (a tEMG signal loss).
- They reported that 3 out of the 15 people who had signal loss also demonstrated vocal paresis post op (none with vocal cord paralysis). Let’s assume that my hunch is correct, and there was some technical errors. Well, the paresis rate isn’t looking so hot. So now you’re risking injury to the other side as well (they did note that there was no signal loss on both sides to any of the patients).
- They showed that loss of triggered EMG signal was restored ~20 minutes after it was lost. Again, not something that I’ve observed at those amounts. There are times when the signal isn’t present after an initial CMAP was produced, but not outside the relatively quick fix of something that is explainable (poor contact, shunting, etc.).
Now, you can see that I don’t take much stock in this study, and don’t plan on making changes to the way we treat our patients. But studies like these are great to challenge what’s currently accepted as “the right thing,” which we know can change at any time. I’d like to see some further proof validating their claims, but for now I’m sticking to a loss of triggered EMG response of the recurrent laryngeal nerve as a significant event that should lead to the postponement of the removal of the other thyroid lobe.
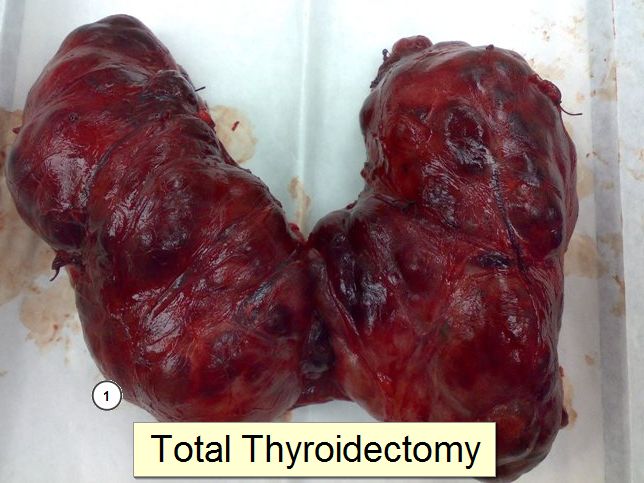
UPDATE: For those doing neuromonitoring and don’t have much exposure to doing thyroidectomies, here’s a video of the surgery. This is a HUGE incision. I guess it makes for a better video…
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...