Saphenous SSEP For Protection Of The Femoral Nerve During Transpsoas Lateral Interbody Fusion.
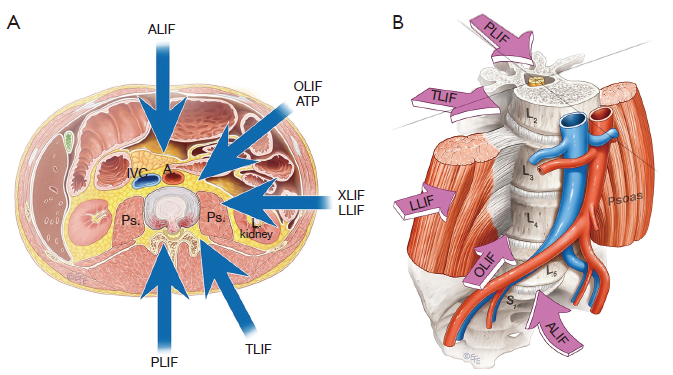
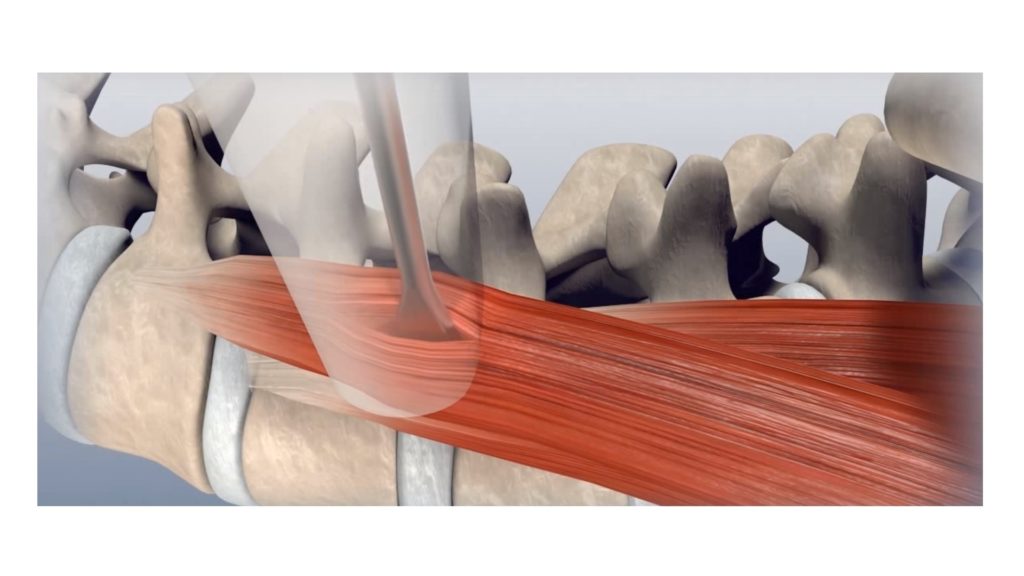
Not too long ago, lateral interbody fusion procedures really started to pick up in popularity. Some large studies came out that showed you could fuse the spine with less incision and dissection size, less blood loss, shorter surgeries and hospital stays, better fusion and the biggest kicker, less pain. One of the risks associated with this procedure was at the level of the lumbar plexus as it is forming the femoral nerve. This sparked the question, “Should we be using saphenous SSEP monitoring in these cases in addition to posterior tibial nerve SSEP, which is there more for spinal cord monitoring?”
Knowing that this surgery type isn’t too old, automated neuromonitoring systems are used in these cases and the fact that we are limited to whatever cases our surgeons book us to work on, it got me wondering how many people have done this type of case. So before we get into the meat of this, let me ask this question:
“Before we get into the technical aspects of Saphenous SSEP, let’s talk about the surgery?”

Transpsoas Lateral Interbody Fusion

“Is there anything else you can offer to monitor nerve compression?”
Saphenous SSEP
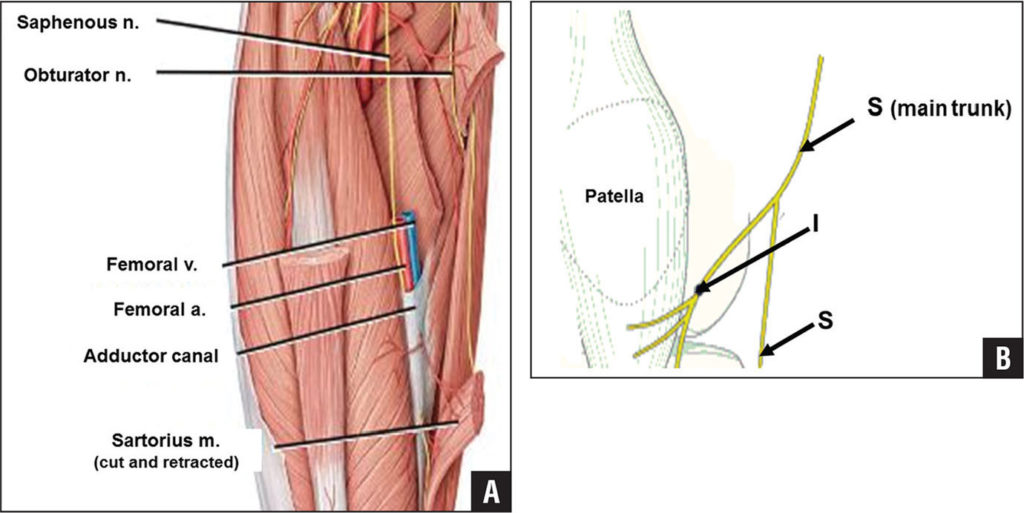
Wait… SSEP are typically not very helpful for lumbar surgeries for monitoring the peripheral nerves. We use it in tandem with sEMG because SSEP in lumbar cases has a high specificity (although low sensitivity) to match sEMG’s high sensitivity (although low specificity). Since this case places the neural structures at risk at the level of the plexus and nerve, SSEP becomes a more sensitive test. Not the posterior tibial nerve SSEP, because the sciatic nerve isn’t the nerve at risk. We need to run it off the saphenous nerve, which is a sensory branch of the femoral nerve.
In order to use this nerve, we need to first understand some limitations.
- First – this is a sensory nerve. Sensory nerves do not have the size and speed of larger, mixed nerves. That means that we should expect smaller amplitudes and a worse signal to noise ratio.
- Second – this nerve is buried. We like to stimulate mixed nerves at their most superficial location. No such luck here. You’re going to have to palpate the intermuscular space between the vastus medialis and sartorius about 2/3 down the thigh.

- Third – did I mention this is deep? Please don’t waste your time stimulating with sticker electrodes. Data acquisition rates for the PTN have been reported in the upper 80’s and lower 90’s. (Silverstein, 2014) reports an 89% baseline acquisition rate (small sample size), so stick to best techniques from the start and you should not have any additional problems.
- Fourth – this is a sensory nerve surrounded by large muscles. Higher intensities (20-50mA) and longer pulse durations (500-1000uS) may be needed in order to stimulate the nerve adequately. This may cause some movement in those muscles. Keep an eye out when you turn on your stimulator.
- Fifth – this stimulation site is proximal to what we are used to seeing in the LE, and it is a slower, sensory nerve. Take this into account when looking for the positive subcortical and cortical responses.
“If SSEP are more sensitive because it is the distal plexus and femoral nerve we are worried about, what about tcMEP?”

tcMEP for transpsoas lateral fusion?
Even less common and/or studied than using the saphenous SSEP for transpsoas lateral fusion surgery is the use of tcMEP with recordings off of the quadriceps. This could be for a couple of reasons.
- tcMEP do not work as well in proximal muscles. We’d be recording off of the quadriceps. This shouldn’t be a deal breaker since tcMEP works well on shoulder surgeries off the proximal muscles.
- Quadricep weakness has been reported in the literature, but not as often as sensory changes. Saphenous SSEP probably covers that better.
- Might need anesthesia to switch to TIVA
- Surgeons hate patient movement. Especially when the patient is hyperflexed and positioned on their side.
Multimodality monitoring does make sense here, it just hasn’t been well established. There are some groups out there monitoring motor evoked potentials on these cases, and they have shared their observations, but I haven’t seen any real numbers put out (doesn’t mean it’s not out there).
What’s your experience?
Anyone have more than 50 cases of saphenous SSEP under their belt that can speak of their experiences? My experience is pretty much what’s reported in the Silverstein paper, except I haven’t been on a case with a change.
If you aren’t yet using this on your lateral cases, are you now considering it?

Joe Hartman
Subscribe to our Awesome Newsletter.
3 Comments
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...








What will be the latency of saphenous SSEP response recorded at cortex?
Like any other nerve stimulated, there’s going to be a range from person to person. And I haven’t seen a name placed on it, like N20, but they tend to land in the mid 30’s.
There have been complications and now a trend at several companies who monitor a significant amount of laterals of using peroneal nerve at the ankle over PTN or CPN during lateral fusions. This nerve is more directly affected with positioning changes. Using the ankle response over the knee, results is less patient movement.