Possible Facial Nerve Monitoring Blunder…
Facial nerve monitoring is one of the things that we as intraoperative neurophysiologist can perform with a high level of certainty Because of the amount of research demonstrating its usefulness, the information we give back to the surgeon is indeed on par with what is happening from a functional standpoint.
To say it differently…this ain’t monitoring EEG of depth of anesthesia.
But there are some fine points to this procedure that I’m not sure everyone performing it is completely aware of… and should be. This goes for the intraoperative neurophysiologist, the remote monitoring physician and the surgeon.
To lead up to what I’m referring to, let’s walk through a typical cerebellopontine angle surgery that has an atypical triggered EMG response while you’re performing facial nerve monitoring during surgery.
Cerebellopontine Angle Tumor Surgery And Monitoring The Facial Nerve
The surgeon has exposed the tumor and retracted the cerebellum out of the way. There is no facial nerve free-running EMG, and your SSEP and BAER are still tracing along with baselines. So far, so good.
The surgeon sees the tumor (it’s pretty big and a bit of a tight squeeze in there), and now it’s time to start identifying structures. S/he wants to be able to decipher the tumor from nerve, as well as get some information as to the functional integrity of the facial nerve.
First the surgeon goes deep and stimulates the trigeminal nerve. You know this because you set up a channel in the masseter, and the latency was about 3-4 ms. Looks good.
Then the surgeon stimulates what s/he thinks is going to be the facial nerve. You’re at 0.3 mA and a pulse width of 100 usec, and you see the orbicularis oris start to fire off at around 11 ms.
Facial nerve CMAP at 11 ms?
That’s odd??? That’s not really the sweet spot for the facial nerve. It usually comes in around 5-7 ms, maybe a little earlier. Maybe it’s because the tumor stretched the nerve, making it a longer trip? Or maybe there’s some compression and the nerve’s conduction speed is hindered?
And look at that… you have the nasalis, orbicularis oculi and frontalis all covered, yet those remained quiet. The facial nerve doesn’t branch till it’s up by the parotid, so you know it’s not that.
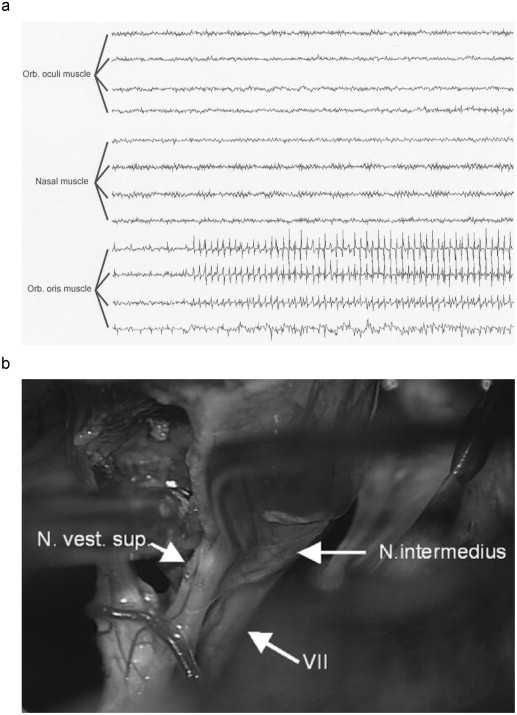
Also, something just didn’t look right in the free-running EMG when it stimulated (you just happened to glance there too). It was a pretty weak response, and it had some larger than normal spaces between the responses. Come to think of it, you’re triggered EMG window looked kind of flat too. The morphology of the wave wasn’t that crisp response you’re used to seeing. The CMAP was low amplitude and longer duration.
Here’s what it might look like, and what the surgeon is seeing at that point…
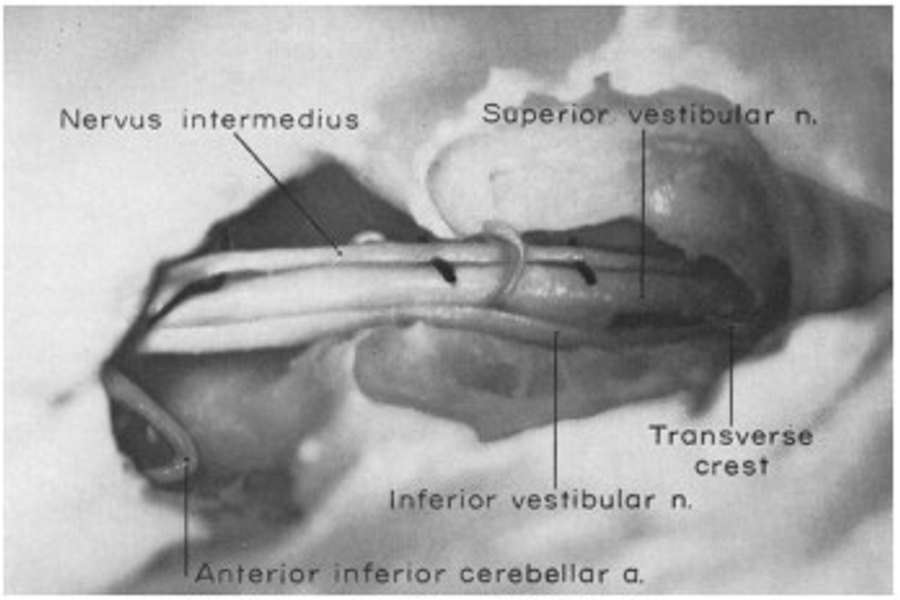
What you’ve seen is not typical for facial nerve stimulation, but rather for nervus intermedius stimulation. While most know the nervus intermedius for its sensory and special senses distributions, it actually has motor fibers to the orbicularis oris too.
If the surgeon has located the nervus intermedius, but because it stimulated the orbicularis oris, s/he might think they’ve found the facial nerve. S/he might find themselves in a predicament. The main trunk of the facial nerve can be in a completely different location of the cerebellopontine angle. If they start debulking tumor under false pretenses, they could possibly cause some facial nerve trauma.
So you step your cranial nerve monitoring game up…
When you see this presentation (a low amplitude, longer latency of just “off” looking morphology that only stimulates the obercularis oris), you need to suggest to the surgeon to continue looking for the trunk of the facial nerve.
Well, that’s a nice little piece of information for you. But what else could you take away from this?
How about this…
The next time you’re doing a cerebellopontine angle tumor case, check to see if there is any motor weakness. If there is weakness (even better yet, they actually did neurodiagnositic studies ahead of time and there was a localized denervation potentials) only in the orbicularis oris, you might be able to “discuss” with the surgeon about how the tumor is probably affecting the nervus intermedius, and that your facial nerve monitoring should help localize that area. That’s very hard for MRI imaging to do (intermediate nerve schwannoma vs facial nerve schwannoma), so you might be his/her eyes on the inside. What a superstar you’ll be!
And if you need a little brush up on facial nerve anatomy, check out Dr.Najeeb
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...