Monitoring Train Of Four During Surgery
From the perspective of the anesthesiologist, one of the benefits of having a surgical neurophysiologist monitor during surgery is a more precise measurement of muscle relaxation or train of four monitoring. In some of the cases, we need to allow the patient to regain a sufficient amount of muscle activity to monitor central and peripheral motor systems (more on how to do that later), while in other cases we are assisting in making sure that the patient isn’t going to move at all during the surgery. At the end of the case, we can also lend a hand to the anesthesiologist to make sure the patient has a smooth wake-up.
Making Sense of Train Of Four And Twitches
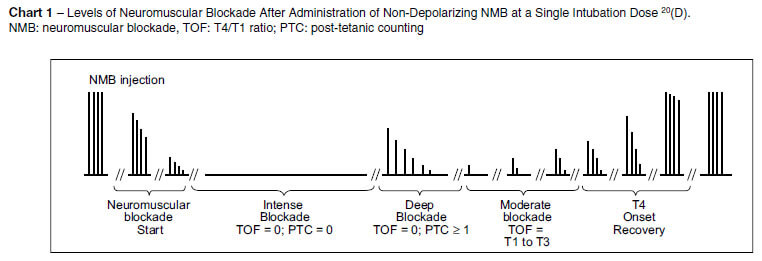
There are a couple ways to monitor the lasting effects of the neuromuscular blockade on the neuromuscular junction. Let’s first go over how to collect them and then how to use it clinically.
T1 amplitude/T1 baseline amplitude
In order to perform this train of four test, you need to be able to collect a CMAP prior to any muscle relaxant given. There are some instances when no muscle relaxation is given, but the typical process of giving an upfront dose in order for anesthesia to place the breathing tube excludes this technique for the majority of cases.
Here you are looking at the amplitude height of the first response in the train of four and comparing it to the first response in any other train of four collected after muscle relaxants have been given. According to (Sloan, 2002), when neuromuscular monitoring is conducted this way, successful monitoring of myogenic responses has been accomplished at T1 between 5% and 50% of baseline.
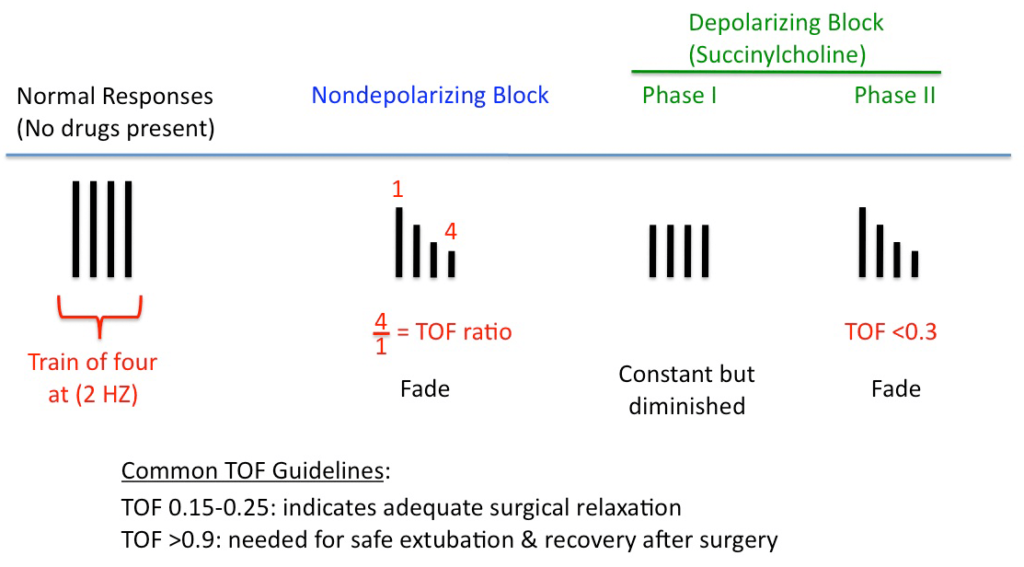
T4:T1 ratio
A more frequently used technique is to measure the ratio of the fourth twitch amplitude (T4) to the first twitch amplitude (T1). This is referred to as the T4:T1 ratio. You do this by setting up amplitude markers on each CMAP from the highest peak to trough for T1 and T4. If T4 does not have an amplitude, then you cannot measure this ratio.
If you are using T4/T1 for tcMEP, use the following as a guide (given in a presentation by Dr. Sloan):
- Only T1 amplitude, no T2, T3, T4… then your CMAP will be about 40% of max amplitude
- Only T1, T2, but no T3, T4… then your CMAP will be about 60% of max amplitude
- Only T1, T2, T3, but no T4… then your CMAP will be about 65% of max amplitude
- T1, T2, T3, T4… now you can start looking at the ratio.
If your T4/T1 ratio is greater than 60%, then you will still be able to get a max CMAP for tcMEP. For example, if T4=600uV and T1=1000uV, then T4/T1=0.6.
So if your TOF ratio is less than 60%, but you still have a T4 amplitude present, then the amplitude of your CMAP should be between 65-99% of max amplitude.
You will notice that a percentage reduction in the supramaximal peripheral nerve stimulation is not equal to the percentage drop of a CMAP from a tcMEP. The amplitude of the CMAP is much larger and more resistant to the effects of neuromuscular blockade, which is why you can see a 100% tcMEP amplitude with only a 60% T4:T1 ratio.
T4:T1 ratio for pedicle screw stimulation
If you are using the T4:T1 ratio for pedicle screw stimulation, some author have suggested a ratio > 80% for optimal results. You can also find authors suggesting you only need 2 twitches out of four as well, but I believe that advice is not as well accepted by most in the neuromonitoring community.
If you were able to get a baseline T1 and were able to use both the T1 amplitude/T1 baseline and the T4:T1 ratio, you might see the following patterns:
- There is a gradual decrease in the amplitudes from T1 to T4 as less Ach is dumped in to compete with the blockade.
- When there is only 1 twitch out of 4, the T1 is less than 10% of baseline T1
- When there is only 2 twitch out of 4, the T1 is less than 10-20% of baseline T1
- When there is only 3 twitch out of 4, the T1 is less than 20-25% of baseline T1
Visual inspection or palpation for twitches
A very gross estimate of how much muscle relaxation is still on board is by looking at the hand or palpating the muscle during supramaximal stimulation. We can also make similar estimates when we run a train of four without a baseline T1 measure or a present T4 to calculate a T4:T1 ratio. We’re kind of in the middle, so we will end up saying something like “looks like we have about 2 twitches.”
But once we do start to get a CMAP on T4, it is a much more sensitive test to perform an actual ratio from the recorded amplitude than to go by feel or visual inspection of the muscle twitch. The greatest weakness of visual or tactile evaluation of the muscle response is that a fade cannot be reliably detected whenever the TOF ratio is greater than 0.4 because all 4 muscle contraction responses are seen or sensed equally at and beyond this range of fade.
Want to become even better friends with anesthesia?
You can offer some valuable information to the anesthesiologist when looking at the train of four response when the patient is awakening for extubation. Several studies have shown that the ratio of the 4th response to the 1st response in the TOF sequence (TOF ratio) should return to at least 90% to ensure full control of pharyngeal and respiratory muscles and to maintain a normal hypoxic ventilatory response. Going just off of visual inspection or palpation leaves you in a range of uncertainty (between 40% and 90% T4:T1 ratio). This may expose the patient to incidences of critical respiratory events.
Monitoring Train-Of-Four When Full Paralysis Is Requested
When we monitor for TOF, we usually are looking to monitor over muscles that are involved in the surgery. For instance, the abductor hallicus brevis makes for an ideal muscle in lumbar surgeries. But sometimes the surgeon has to deal with a large exposure and tight muscles. They may end up requesting that the patient has 0/4 twitches. Knowing that the more proximal muscle groups are more likely to be resistant to neuromuscular blockade, we may elect to monitor one of the hand muscles. Or the anesthesiologist (or us) might set something up off a facial muscle.
But distal vs proximal isn’t the entire story here.
We need to look at the type of muscles we are monitoring. The hand muscles are typically used for fine movement and contain mostly fast twitch, striated muscles. These are used to produce a brief burst of tension (like when typing). If more force is required (hammering a nail), the increase in force is accomplished by recruiting more muscle fibers (really motor units). These highly precise movers have a very small innervation ratio (1:200), meaning that each motor unit supplies few muscle fibers. This is not the same in muscles that function primarily for gross movements or stabilization.
Pro Tip: This low innervation ratio is one reason why the hand and feet muscles work so well for tcMEP. In a proximal muscle that has a larger number of muscle fibers monitored per motor unit, a drop-off of a few motor units can result in a large drop in CMAP amplitude size if you compare that to the drop off in one motor unit with a smaller innervation ratio. That makes it harder to collect a reliable response, and may lead to false positive calls if selecting too restrictive of an alarm criterion.
But back to selecting muscles for train-of-four monitoring…
Facial muscles, on the other hand, are slow twitch muscles used to express emotions and non-verbal communication. They can sustain a high level of tonic activity with subtle changes in contraction force.
Despite these and some other differences, the muscle testing for train-of-four has been generally accepted as the same when testing the facial muscles and muscles of the hands. But they probably shouldn’t. While the variability between responses over a large group of people makes it impossible to predict responses from the hands vs the facial muscles in train-of-four testing, the muscles of the face are generally more resistant to muscle relaxants.
Guess what other muscles are more similar to these slow twitch muscles that are used for tonic activity (like standing upright)?
Here’s a hint: it is the same group of muscles that the surgeon is fighting with during exposure.
Here’s another hint: it is the group of muscles that are in the exact proximity of these high current cutting devices that activate the muscles and make them jump.
Yes, it is the erector spinae muscle. And in cases where the surgeon is requesting 0/4 twitches, using the facial muscles makes much more sense than a distal muscle used primarily for fine motor skills. Facial muscles are more resistant to the effects of neuromuscular blockage drugs. This diminished sensitivity may be due in part to their lower innervation ratios.
At the same time, if you are just monitoring the facial muscles, then you need to be cautious as to not overdose the patient with muscle relaxation. Considering this fact, then it makes sense to monitor the hands or feet as well.
Last but not least – CYA
The one word I’d like to stress in the above paragraph is the word “assist.” We are there to set up and monitor motor responses, but we are not there to dictate on how to prescribe the medical treatment. The best and the only way to monitor the anesthetic effects of neuromuscular junction is to report the quantitative numbers from our train of four recordings to the anesthesiologist and/or the surgeon and allow them to make a decision off of all the information presented.
In my own case notes, I make sure to verify my role in the operating room when it comes to monitoring twitches. Here’s an example note (abbreviations were explained earlier in the note):
In the Setup portion of the note:
TOF monitoring was conducted as an adjunct to anesthesia’s own assessment of muscle relaxation and visual observation of the movement of the extremities during SSEP stimulation. Four monophasic, rectangular pulses were delivered by a constant current stimulator at the left wrist over the ulnar nerve and left ankle at the posterior tibial nerve. CMAPs were recorded over the first dorsal interosseous on the left hand and abductor hallicus brevis of the left foot.
In the baseline assessment:
A TOF of 4/4 with a T4/T1 ratio of 65% was recorded prior to incision to assist the anesthesiologist/CRNA in determining the appropriate level of muscle relaxation.
As you can see, I am clearly defining my role in monitoring the patient’s level of the anesthetic blockade on board. And there is nothing false about that statement. Our scope of practice does not encompass assessment and administration of anesthetics. I run a train-of-four every 30 minutes, whenever asked by a member of the surgical team, whenever asked by any remote oversight or whenever appropriate to the procedure… and then relay the findings.
Why am I harping on this point? Because when things go bad, index fingers get pointed. If the patient moves when the surgeon isn’t expecting it, should the surgical neurophysiologist be the one blamed?
It happens, but it shouldn’t.

“If you didn’t document it, then it never happened!”
So just like covering yourself with appropriate documentation, you should also cover yourself with the conversations you have in the operating room. Let the anesthesiologist know that you are running train-of-four periodically so you can make sense of the neuromonitoring. If they would like you to run it at any point during the case so they can better assess anesthetic levels, please ask and you will give tell them what the numbers show.
And when you do have those conversations, document all of them in the event log.

Joe Hartman
Subscribe to our Awesome Newsletter.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
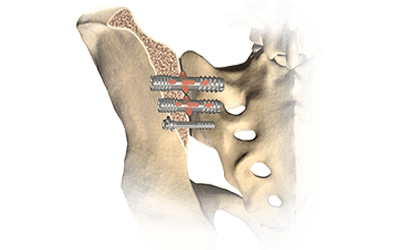
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...




0 Comments