Direct Motor Evoked Potentials
Continuing on from the post about intraoperative monitoring for gliomas (and trying my best not to ramble on too much in this post), I’d like to discuss some pros and cons to using a surface electrode strip as an anode directly on the motor cortex with a cathode at F1/F2 or Fz for direct motor evoked potentials.
Performing dcMEP with a surface electrode has been used with great success in reducing postoperative deficits. It’s been successfully used in various brain tumor, cyst and arteriovenous malformations to help reduce morbidity rates.
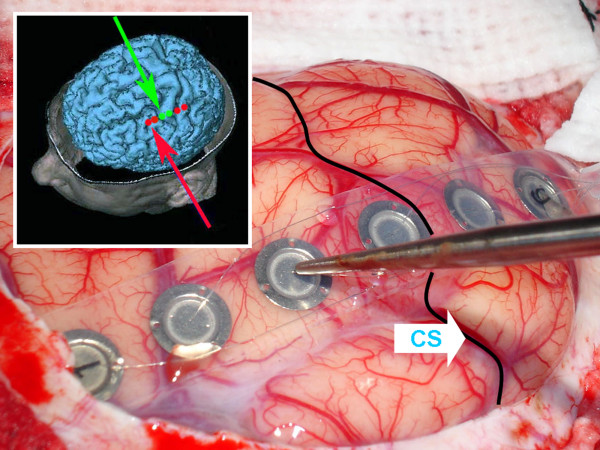
Most surgical applications of this technique follows the original work of Taniguchi (1993), where a strip electrode is placed over the motor strip and uses a high frequency anodal square wave pulse. This electrical impulse stimulates the primary motor strip, including Betz pyramidal cells, to transmit motor activity along the corticospinal tract.
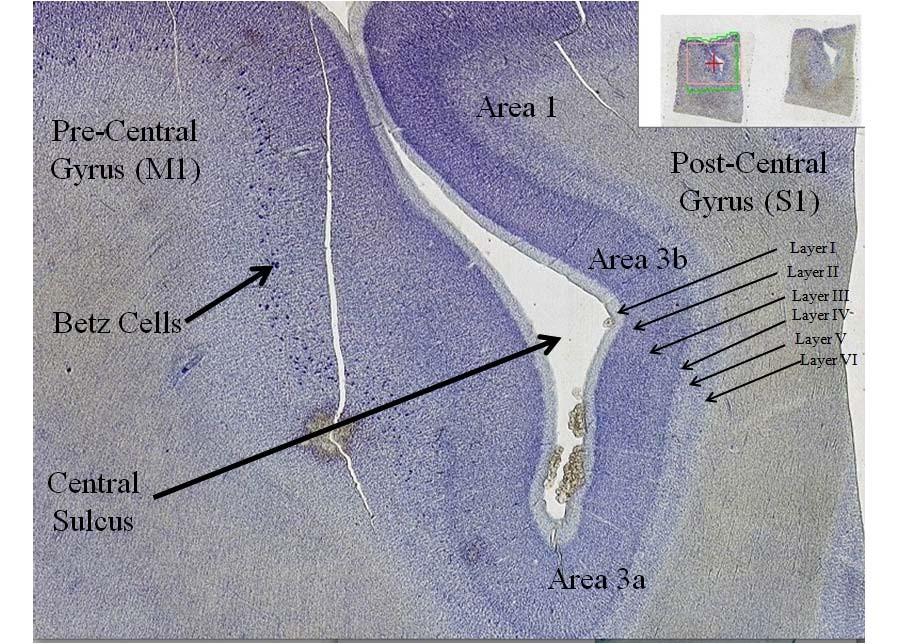
Image from http://bit.ly/128FvhT
There are a number of studies that describe the pros and cons of using an electrode strip for direct cortical MEPs. Here’s a summary:
Pros
- Can produce reliable CMAPs at low intensity (<25mA) and no patient movement. Set it up on a timer and let it go.
- Can monitor semi-continuously throughout the craniotomy, possibly giving early warning for surgical intervention
- Even though shunting/spread is a concern due to monopolar stimulation (could stimulate the corticospinal tracts directly, so deficits in the cortex could go undetected), the false-negative rates are low. This has been attributed to the lower intensity stimulation.
Cons
- Electrode is bulky and can be in the way
- Monopolar stimulation does not allow for the most reliable mapping of the motor strip
- Requires TIVA and no muscle relaxant
- Cannot be used in kids under the age of 2 (incomplete myelinization of pyramidal tract)
- Cannot be used on people with less than 3/5 muscle strength
- Inadvertent change in electrode position can affect CMAP
- Fluctuations have been observed and attributed to complexity of motor system
Final note: I’ve done them by manually switching the electrode in the pod, as well as using a switch box. Both have worked great. Just make sure to find the best response at the lowest stimulation level possible.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...