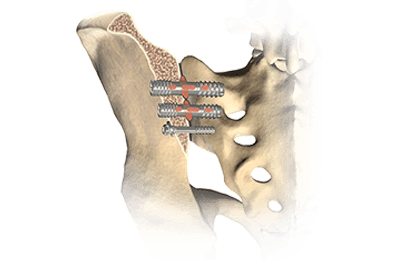
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring
EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the option is available to surgeons using nerve monitoring for their lumbar cases.
But knowing the difficulty of identifying sacral foramen on imaging and the variations seen in sacral bones, it made me wonder why nerve monitoring would not be used more often. It seems that it could be as useful, or even more useful, during the searching phase when placing the implant than even than just stimulating the final position. If the surgeon’s visual guidance is reliant on less than optimal conditions, adding in this physiological test should allow for the surgeon to make a more informed decision.
So I went hunting for an article in hopes to find something useful and came across the following article from Woods et al.
Woods, M., Birkholz, D., MacBarb, R., Capobianco, R. and Woods, A. (2014). Utility of Intraoperative Neuromonitoring during Minimally Invasive Fusion of the Sacroiliac Joint. Advances in Orthopedics, 2014, pp.1-7.
Their Findings
Right off the bat… yes, this is a small, retrospective study. But I do like how they are using nerve monitoring through different stages of the implantation process. The intensities used were created by looking at animal studies and stimulation intensities used for EMG nerve monitoring in lumbar surgeries, but are probably best guesses and seemed reasonable to me at this point in time.
In their findings, they stated “111 implants resulted in 8 true positives, 3 false positives, 2 false negatives, and 98 true negatives. These results provide sensitivity and specificity rates of 80% and 97%, respectively.”
But if you look at the descriptions of the false negatives and false positives, there are lessons to be learned there. For the false negatives, the first case demonstrates the usefulness of EMG nerve monitoring in a “searching” mode to better identify problems. The second case is questionable to point to the EMG nerve monitoring as the problem. For the 3 false positives found in the single patient, the limitation of EMG nerve monitoring in that patient was very real. As it turns out, there seemed to be an anatomical variant
For the 3 false positives found in the single patient, the limitation of EMG nerve monitoring in that patient was very real. As it turns out, there seemed to be an anatomical variant causing a problem in the sensitivity of the modality. Knowing that this surgery is in an area where anatomical variations are not uncommon, the surgical neurophysiologist and surgeon would be able to make a better judgment of the recordings as it relates to their other measures (fluoroscopy, experience, etc) and tilt towards a greater reliance on those in cases where there is a known variation that might cause a challenge to EMG nerve monitoring (like dysplasia).
While I wish the author would have gone into a little more detail on the false negative cases, and I really wish they were able to include a larger patient population, the paper did give some guide to utilizing EMG nerve monitoring for minimally invasive sacral iliac surgery that I hope will spark further study and implementation.
Minimally Invasive Surgery Video
For those less familiar with the surgical procedure, here’s a video of one type of minimally invasive system to fuse the sacroiliac joint:
How about you – are you utilizing EMG nerve monitoring during this case type? Care to share your experiences?

Joe Hartman
Subscribe to our Awesome Newsletter.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Surgical Neurophysiologist Salary: Who Are The High Earners? Part 2
In Response To High Earning Surgical Neurophysiologist Being The Best At Sales [Joe's notes: This is a guest post - or really a response to my previous post - that was insightful and, well, long enough to turn it into its own blog post instead of a comment. Full...
Surgical Neurophysiologist Salary: Who Are The High Earners?
Surgical Neurophysiologist Jobs That Pay Looking back over the past decade of money being paid to a neuromonitoring technologist, there's been some waxing in waning in the surgical neurophysiologist salary category as to who deserves the higher salary. 10+ years ago,...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...





0 Comments