Muscle Relaxants And Neurophysiological Monitoring
So you want to tell anesthesia they can’t use muscle relaxant on this case? You’re bound to get a wide ranges of responses, from acknowledgement, dirty looks and maybe even a full blown temper tantrum. It’s helpful to go in with a little understanding of how muscle relaxants affect our monitoring to clearly state your reasoning.
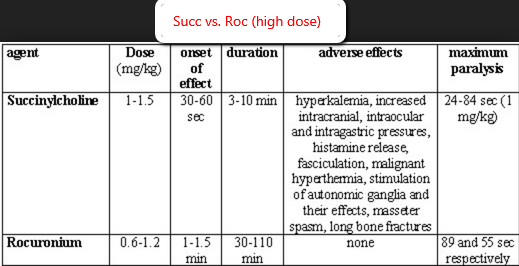
The drug of choice around my area is rocuronium. It’s a non-depolarizing muscle relaxant that doesn’t take all day to wear off, and doesn’t take too long to take effect. Intubation is smooth, patient positioning is smooth, they can keep the patient from moving during surgery, they’re good at timing their wake up to give a little neuro exam shortly after and the patient doesn’t wake up with muscle soreness (or run risk of malignant hyperthermia or hyperkalemia like what can be seen with succinylcholine). Thumbs up all around.
But there are some cases where you’ll need full twitches (ok, some will argue 2 or 3 twitches should suffice) right away. This might be in a tcMEP case, thyroidectomy with NIMS tube neuromonitoring, minimally invasive, peripheral nerve cases, etc. Our options then become a small dose of non-depolarizing, depolarizing (succinylcholine) or nothing at all.
Planning The Use Of Pre-induction Muscle Relaxant With Anesthesia
First off, we need to be realistic as to when we actually need to test what we’re testing. If we’re taking tcMEP baselines in a stabile patient (not worried about positional problems), we might be able to go 30 minutes before we need to set our baselines (with all the setup and prep being done). If we’re doing prepositional tcMEP for a trauma case going prone, then we’re going to need full reversal about 10-15 minutes after induction (depending on how many channels you’re running and how much you can get done before the nurse tries to put in the foley). If you’re monitoring with a NIMS tube, then you’ll want to test muscle activity in less than 5 minutes of intubation.
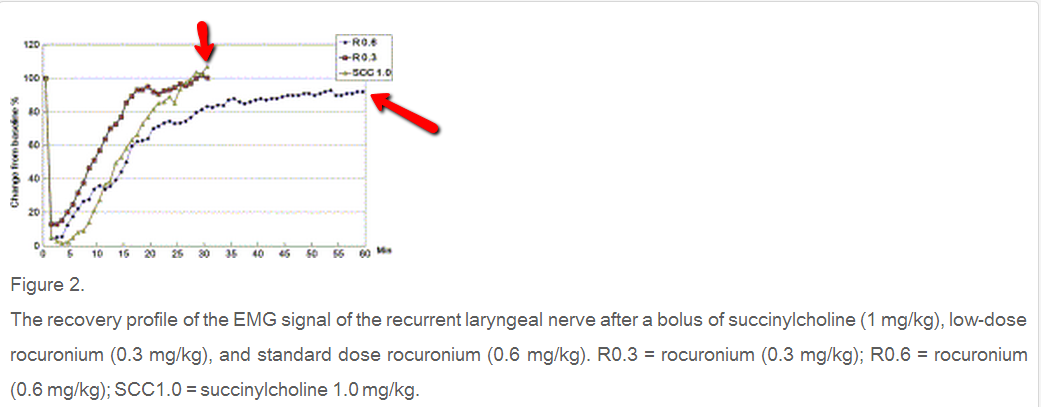
Next, we need to compare those realistic times with the duration of medications. Rocuronium (also called zemuron) has a significant does response effect on recovery time. A recent paper (A comparison between succinylcholine and rocuronium on the recovery profile of the laryngeal muscles during intraoperative neuromonitoring of the recurrent laryngeal nerve: A prospective porcine model) showed that a low dose (0.3 mg/kg) of rocuronium recovered 80% in 15 minutes, with full recovery in 30 minutes of the laryngeal muscles. A 0.6 mg/kg dose of rocuronium reached 80% recovery around 30 minutes, but took greater than 1 hour to recover 100%.
What’s surprising to me was their findings comparing low dose rocuronium and 1.0 mg/kg of succinylcholine. The low dose rocuronium was around 5 minutes faster to reach 80%recover, and was at 100% recovery, it was about the same time (30 minutes). I typically associate succinylcholine as the necessary evil to get up-front baselines ASAP.
Wouldn’t it be nice to not have to restrict anesthesia to using succinylcholine for anything? But I’m not sure that’s how things are. A low dose is fine for baseline tcMEP before incision, probably not a great idea if you’re getting pre-positional baselines (unless everyone is aware it might take a little longer to wear off and are willing to wait it out), and most likely not a good option during thyroidectomies using a NIMS tube (since you want to get impedances checked and muscle activity recorded before they tape the tube). But at least now you have some numbers to give them as to what qualifies as a “small dose of roc up front.”
If they absolutely can’t intubate without muscle relaxants or using succinylcholine, then maybe the tube shouldn’t be used, but rather needle insertion into laryngeal muscles.
Please Note
*** The article used for the clinical numbers should not be taken as gospel. This was done in a porcine model, and was monitoring muscles that are well known as some of the first to recover from muscle relaxants. Neurophysiological monitoring of transcranial motor evoked potentials in an adult abductor hallucis brevis may not necessarily correlate with a pig’s voice box.***
[socialpoll id=”2365146″]
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...








Thank you for the Anesthesia Muscle Relaxant tutorial, however, you lost me at the “Puppy Dog Eyes” statement. This comment is derogatory and insinuates that the proper Anesthesia Protocol for the patient is decided by the Neuromonitoring Technologist using “Puppy Dog Eyes”.
Also, in order to be taking seriously, please provide your data references and Intraoperative Neuromonitoring Credentials.
Thanks for reading Margaret. I’m sorry I lost you at the second sentence (which has been changed). Using a term like “puppy dog eyes” was in no way intended to insinuate manipulating anesthesia to get your way instead of following proper Anesthesia Protocol.
That being said, this is the blog section of the website, where I try to inject some (poor) humor into the topics. Here you will find opinions, rants, advice, musings, puns, tongue-in-cheek remarks and maybe even a bit of controversy. I believe that’s on par with socially accepted standards for a blog.
Data references can always be found by hyperlinks pointing to the published data in each of the blog post.
My credentials are listed in my author bio at the bottom of every post ever written, as well as in the Meet Joe Hartman section found at the header.
Thanks Joe. I have found your posts to be very informative and I continue to share them with our colleagues.
Your blogs are well referenced and presented in a unique way that makes them easy to understand and even enjoyable.
Keep up the good work Joe. Don’t change a thing. And, thanks for your support of our profession.