Recording Electrodes For EMG in the Operating Room: Referential or Bipolar?
If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do this to everyone I work with (in a nice way of course). It’s a great exercise, especially when you do this with topics that are still in a gray area. Intraoperative EMG lives in that space.
There’s a different level of understanding when you have thought through your reasoning instead of regurgitating your company’s policy and procedures. That’s why it is a great idea to start up these types of conversations.
I’ll debate myself by taking different sides of the argument. Please feel free to add to the discussion and take a side yourself.
Joe Defends Bipolar Intraoperative EMG
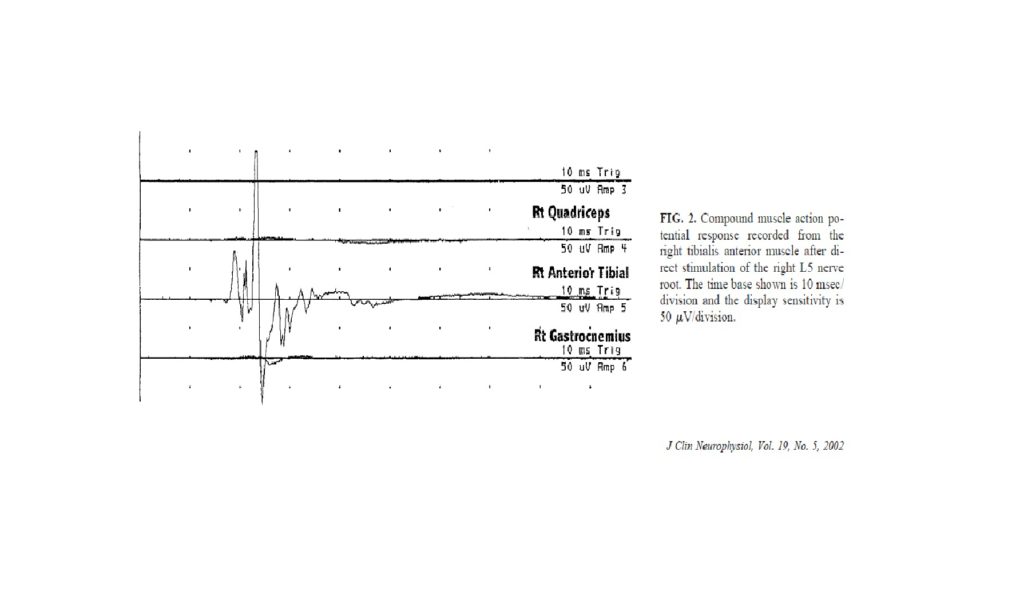
I realize that out of the hundreds of thousands of IONM cases done each year, I’m only aware of a very small fraction of the cases. That being said, I believe that most of the profession is using the bipolar set up for intraoperative EMG. The main reason being that you can help isolate nerve roots for the surgeon by relaying which muscles had a compound muscle action potential with stimulation, what the amplitude size of each was at different stimulation intensities and which muscle has the lowest threshold.
If you look at the Holland, 2002 paper he says… “most muscles receive co-innervation from two or more adjacent nerve roots, and accurate localization of nerve root irritation and/or nerve injury can be obtained only by monitoring multiple muscles simultaneously.” So if you’re monitoring the deltoid and biceps, and you get a response in both muscles, you’re probably at C5. If you’re getting a response at only the bicep, you’re probably at C6. The same thing could be said if you had the surgeon stimulate each nerve root with a hand held probe.
There used to be limitations placed on the surgical neurophysiologist by the number of available channels. Most systems have 16 to 32 channels available now. Unless you’re doing a scoliosis or brainstem surgery, you probably won’t have those restrictions placed on you. If you are put in that position, you really need to find out what needs the most attention. In a scoliosis case, we’re really interested in the spinal cord, so SSEP and MEP, and pedicle screw placement. In order to monitor all of that, you’ll probably have to split your electrodes.
I’ve even had to use an extra pod on the Cadwell before. It was programmed that the B pod was always EMG. When the surgeon was working in the upper thoracic, the EMG was split in the intercostals and upper abs. When the surgeon got past that level, I took out that pod and plugged in a separate pod into the B pod input that had EMG for the abs and lower extremity. That allowed us to watch EMG and test screws with a referential setup, have enough channels to have bipolar MEP recordings in the lower extremity and enough channels for SSEPs. But that is out of necessity to best monitor that case with the limitations given. I wouldn’t carry that over to a L4-5 fusion, since that isn’t the best monitoring available.
Joe Defends Referential Intraoperative EMG
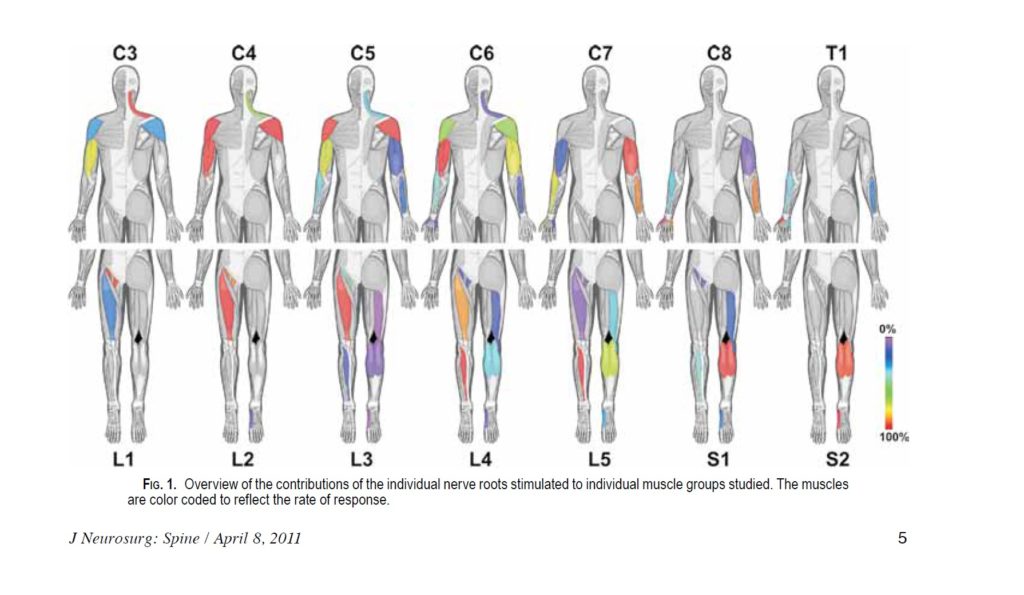
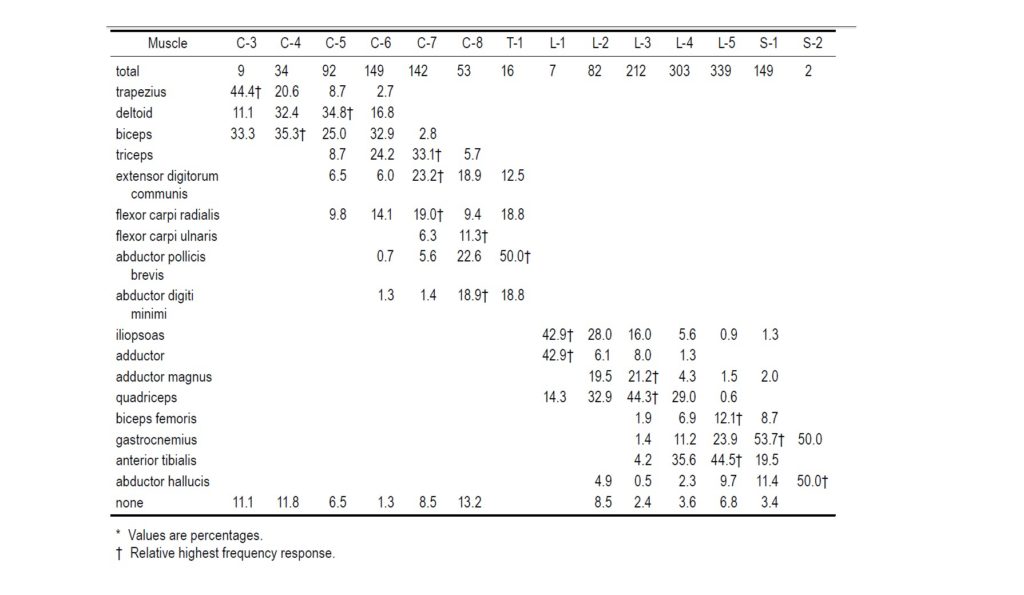
The first thing I always hear about why NOT to do referential recordings is because you can't tell the surgeon which nerve root they are stimulating by the muscle being activated. But I feel that most people are overestimating the actually improved specificity seen by using a referential montage over a bipolar montage. In the extremities, there is just far too much inter and intrapersonal variability. It would be nice if our anatomy was exactly as drawn out in Netter's anatomy book, but it never seems to work out that way. A study done by (Whittenberg, 1998) showed no correlation between MRI findings and clinical presentation of the nerve roots in lumbar spine surgery. So there shouldn't be any preconceived notion as to what should or shouldn't be problematic. If you look at (Schirmer, 2011), they demonstrated a very wide distribution of nerve root innervation that varied greatly from what we are taught to expect. If you just look at the graph they made showing muscle responses, on average, after that root has been stimulated. It is hard to say that the if you get a response from the tibialis anterior, then you're at is L5. It can span from L3 to S1. On the flip side of things, you can't say that you should see a deltoid on C5 stimulation, but not C4. That's just not the case.
Look at the tibialis anterior. It can range from L3-S1. See anything else different that what you've been told?
What about using a threshold to help identify the nerve root with supreme specificity. If we see a bunch of response and turn down our stimulator to till the last muscle shows a tiny CMAP, then some might hang their hat on verifying the root level by the muscle showing the response. Schirmer's other chart told a different story.
Wait - what nerve root supplies the bicep the most? Who said C4? And aren't the adductors used in isolation to isolate L2?
If you had a muscle that is supposed to be mostly innervated by a certain nerve root, you would expect to see those percentages getting close to 100. But I see some that are split almost evenly across multiple nerve roots. And there are some winners that aren't expected, like the bicep having the C4 stimulation bringing it to the lowest threshold the most often.
The second thing I hear is that they don't want all the interference that comes along with electrodes placed far apart. I’m aware that when you increase your interelectrode distance, you are more likely to pick up noise. It makes sense because your electrodes are no longer seeing extraneous noise from the same location, making common mode rejection less efficient. But anyone that has done a number of cases with a referential setup realizes that the noise pickup is minimal at best. But when you consider that the amplitudes from monopolar EMG signals are larger in size compared to bipolar EMG signals, you’re losing out on any benefit of reduced noise since these larger amplitudes will stick out more from baseline recordings. In a bipolar montage, we can expect the amplitude of the close paired recording electrodes to be smaller as some of their signals will be common to both inputs and this is reflected by the differential amplifier. This reduction in sensitivity mitigates any advantage in noise reduction.

"Can you explain a little better how your electrodes actually pick up physiologic activity?"
What An EMG Is Actually Recording
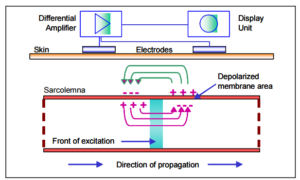
Now, an endplate potential cause sodium to influx for a short period of time causing membrane depolarization and soon after repolarization as ions are actively pumped out. The intraoperative EMG signal is elicited from the AP at the muscle fiber membrane going through this process of changes in electrical charge from the depolarization/repolarization. Once the started, the electrical activity travels across your recording electrode around 2-6 meters per second.
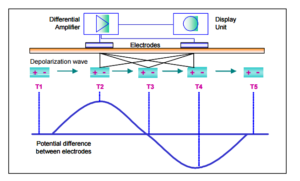
As this depolarization and repolarization along the surface of the muscle fiber approaches and passes your recording electrode, you will see opposite phases in your recording EMG due to the polarity of the dipole and position of the recording electrode.
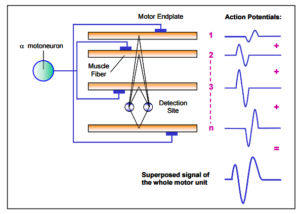
Because the motor unit innervates multiple muscle fibers, and because multiple motor units are typically depolarized at a single time, you will typically see multiple muscle fibers giving off electrical activity at similar times. This electrical activity comes from various distances to your recording electrodes, with less powerful signals coming from a more distant activity.

"What does the distance between the electrodes have to do with it?"
If you place both your recording electrodes in close proximity to one another (1-2 cm suggested), it will be close enough to collect activity from those close neighboring muscle fibers, but distant enough that the signal is not seen as "the same."
While the close proximity of the source (the muscle fiber) and the recording electrodes helps allow for collection, it does not completely prevent some signals being filter out by being too common by our differential amplifier. This is why bipolar signals are typically smaller and have a higher threshold compared to electrodes with more space (worse sensitivity).
But the bipolar setup also does a better job of getting rid of noise from interference. Since there is typically an increase distance from the source (the bed, the scope, the lights, etc.) and your recording electrodes, the signal is seen as "the same" from both electrodes. It is then filtered out. For this same reason, bipolar setups will also help reduce "cross-talk" from electrical activity coming from neighboring muscle fibers. If you've ever tried to monitor muscles from the trigeminal nerve and facial nerve at the same time, you know the importance of using bipolar setups.
What About The Referential Electrode?
The referential intraoperative EMG setup has a larger pickup area than the bipolar setup. This means that the electrodes are spaced far enough apart that it doesn't see the noise coming from a distant source as something completely the same. So it is not as efficient in reducing/eliminating it. At the same time, the larger pickup area allows it to collect more distant physiologic muscle responses, making signal amplitudes larger and CMAPs present at lower thresholds. By placing the electrodes in an active muscle and a distant non-active muscle, you are recording off the electrode over/in the muscle and using the reference to measure against.
"My colleagues do outpatient neurodiagnostics. They record their muscle potentials by placing an electrode over the muscle and the other over the tendon of the same muscle. Why are you doing it different for intraoperative EMG?"

Where part of the muscle gives the best EMG responses?
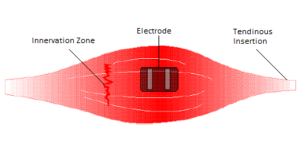
It is typically recommended to place recording electrodes in the middle of the muscle belly, more specifically, in between the motor unit or "innervation zone" and the tendon. This is where there is the greatest amount of electrical activity due to the fact that there is the greatest amount of muscle density. This allows for the recording electrodes to pick up more of the same electrical activity from the same motor unit, taking advantage of a superimposed signal.
That means 2 electrodes, 1-2 cm apart, right smack in the middle of the muscle for a bipolar setup.
For referential, it is recommended to stick one active electrode in the middle of the muscle belly, and the reference electrode (which is also active) in a distant, non-active location. Stick it in another muscle, stick it over a bone, whatever.
What about a hybrid setup?
Placing both electrodes towards the ends of the muscle, or over each innervation zone, has been proposed in the past. This showed to have less bad responses.
There has been a recent resurgence of testing one electrode in the muscle belly and one around the myotendinous junction (not in the tendon). The one electrode takes advantage of the high density, overlapping electrical activity, and the other acts as a reference electrode with greater distance between the recording electrodes that might still be able to still pick up some electrical activity. This was supposed to be presented on a poster at an ASNM meeting, but I haven't seen it out yet.
Your thought?
If you haven't already, go back up and vote on the video, and then let me hear your stance in the comments section below. Let me know why you do things the way you do. I'm going to allow time for the comments to stack up before letting everyone know how I practice.
Want new articles before they get published?
Subscribe to our Awesome Newsletter.
5 Comments
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...
MEP Loss With Levetiracetam: Another Anesthetic To Consider With Motor Evoked Potentials
Levetiracetam And Its Effects On Transcranial Motor Evoked Potentials During Surgery Levetiracetam (AKA Keppra) It's pretty widely accepted that inhalational agents and muscle relaxants will reduce the effectiveness of transcranial motor evoked potentials during...
Help Spread The Word. Social Media Works!






Ok, I understand the concept of the differential amplifier and the issue of noise as it could increase as a function of interelectrode distance. Me, I always use bipolar. Why, because I want those leads over the “belly” of the muscle. Yes, I know anatomically there are instances where the muscle may have innervation from different levels since as you note, not everything anatomically is the same as a Netter textbook illustration. Knowing there may be variation in CMAP amplitude and response at a level that is stimulated for instance in pedicle screw testing, I would want to know the level that is being stimulated is where I expect to see a response. I don’t want an average of what might be a referential response. I can only speak for myself, yet if I am consistent in my placements, I have more confidence that the responses I anticipate are those I expect and can communicate with a surgeon.
I think the problem becomes how to accurately determine what you should see when a nerve root (or pedicle screw) is stimulated is what is happening on that patient on that specific nerve root. If running a bipolar setup and you see a response in the tibialis anterior when stimulating L3 at 6mA, but no response in the quadricep till 8mA, what should the surgeon be told? I think there is evidence that begs to question if going off of what is expected, you could end up wrong as much as you’re right… and sometimes more.
This debate brings forth an issue I have given so much thought to………the benefits of working with physicians in a clinical setting doing EMG first before going into the OR. OK…maybe that is another debate. I personally would choose a small amplitude response that is stable over hours of surgery vs a referential recording that is higher in amplitude but unstable because of artifact requiring more averages. Increased averaging can delay response time to the surgeon. (mostly because you are praying the amplitude will not drop 60% because of some transient artifact; IOM can be a religious experience).
I’m assuming you’re applying this debate to modalities outside of EMG? I think at that point you have other goals to consider.
Joe, this site is excellent. Please keep it running. We need this in the IOMN field.