Spinal Tumors That Need Dorsal Column Mapping
Intraoperative neurophysiological mapping of dorsal columns isn’t really one of the neuromonitoring community’s “bread and butter” cases. Not that there isn’t anything of benefit we offer the surgeon, but because intramedullary spinal cord tumors a pretty rare. The 2 most common tumors that need dorsal column mapping are astrocytomas (seen more in kids) and ependymomas (seen more in adults).
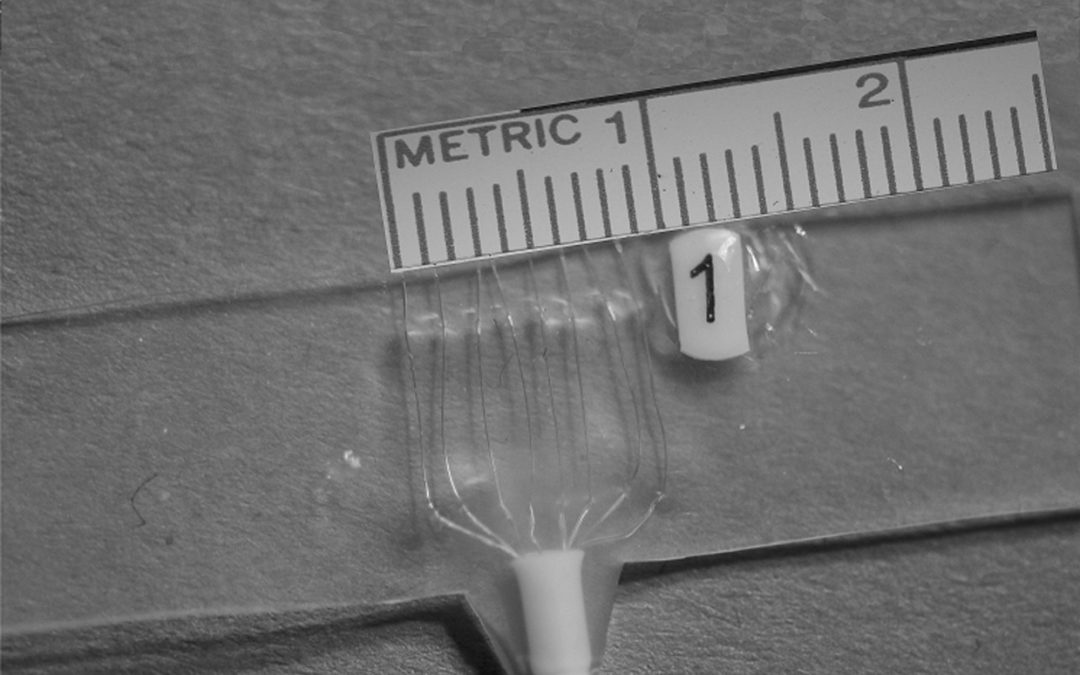
Another reason neuromonitoring companies aren’t marketing our services for these surgeries is due to the expensive electrode used in these cases. There are a couple of versions of the electrode out there, and the one I used was custom-made.
Custom-made = big $$$.
The electrodes have a shelf life, so it’s not unthinkable to order a couple of these electrodes and never use them. (UPDATE: Adtech no longer makes these electrodes for dorsal column mapping. I have no real proof, but it is probably because it was not a money make for them or neuromonitoring companies. There are different techniques available to do dorsal column topography that are much, much more cost-effective).
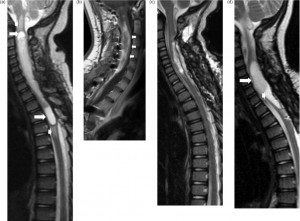
But none-the-less, mapping of the dorsal column will help the surgeon find the midline of the posterior cord to perform the myelotomy. The reason this is of help is because the space occupying lesion will rotate and distort the spinal cord.
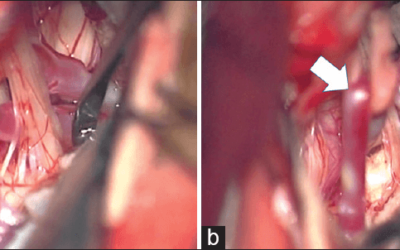
The surgeon uses landmarks, like splitting the elevated dorsal column, to find the midline dorsal median sulcus. The surgeon uses the dorsal median vein as an option to enter the midline raphe and help localize the midline cord.
But edema, scar formation and increased vascularization feeding the tumor ruin their landmarks. And that is we come in.
Dorsal Column Mapping: Setting It Up
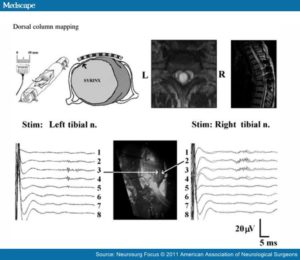
Much like lower extremity somatosensory evoked potentials, we stimulate the posterior tibial nerve at the ankle. The surgeon places the sterile recording electrode (like the one at the top of this post) intraoperatively over the exposed spinal cord. The reference is a sterile needle in a nearby muscle. Placing the electrode perpendicular to the posterior columns allows us to determine where midline is located by assessing the largest amplitude to the ipsilateral SSEP stimulation. The largest amplitude number is recorded and compared to the numbered recording wires running parallel to the dorsal column. Once completed on both the right and left leg, the surgeon knows that midline is between the largest waveform on each side.
In the picture above, the surgeon looks between the 2nd and 3rd numbered wired on the spinal electrode, since those 2 numbers had the largest amplitude. Why are they larger? Because those recording electrodes are more near field to the very midline posterior columns carrying the sensory information.
After Mapping of the Dorsal Column Is Complete: MEP, SSEP, D-Wave
Now that the surgeon has located the midline, it’s time to perform the myelotomy and then remove the tumor or cyst. But you’re not done reducing morbidity rates just yet. Now it’s time to go from mapping to monitoring for prevention of injury. Using 50% reduction in SSEP, 30-50% reduction in D-wave and significant reduction to a loss of motor evoked potentials makes for excellent multimodality monitoring of spinal cord during the spinal cord cases.
And that’s a quick synopsis of mapping the dorsal columns. If this is a new surgery type for you, watch this video of a surgeon I used to work with performing a spinal cord tumor removal with a laser (although he wasn’t using dorsal column mapping in this procedure)
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
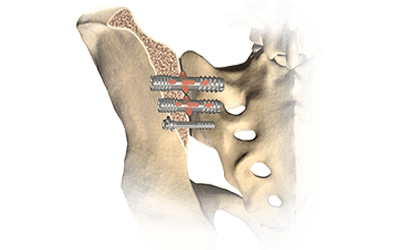
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...