SSEP Increased Variability vs. Increased Latency: A question from a reader…
In my last post, I talked about using the waterfall function to better determine your SSEP baselines, as well as how using it can be helpful in determining your level of confidence with the evoked responses. There was some confusion as to what was being said about speed of conduction vs. latency as it pertains to SSEP variability. So I wanted to clear things up a bit.
SSEP Latency
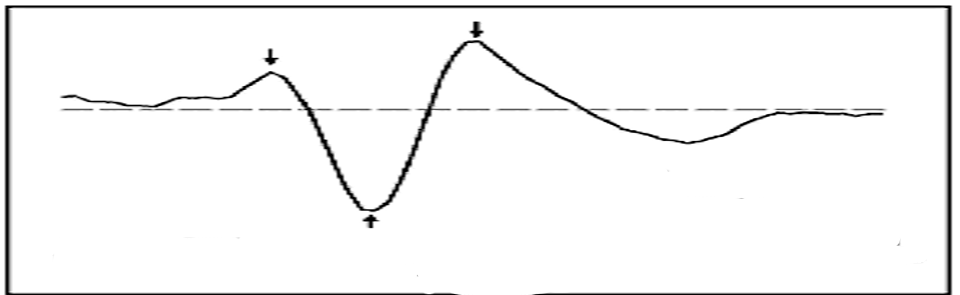
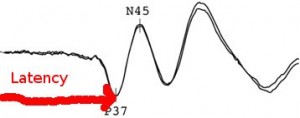
When we look at the latency of somatosensory evoked potentials, we are looking from the stimulus onset to the beginning of the initial deflection.
Reviewing the literature, there’s plenty of physical attributes and diseases that will prolong a SSEP latency. As an example, I stated…
“…the motor conduction slows by 0.4–1.7 m/s per decade after 20 years and the sensory by 2–4 m/s”
For simplicity sake, I’ll continue to use age of the nerve as a factor affecting the trial-to-trial variability of SSEP.
First Things First
So let’s talk speed of conduction, since we’re looking at the initial deflection after the stimulus onset.
If you stimulate over a sensory nerve (like the sural nerve), you’ll see more of a prolonged latency than if you stimulate over a mixed nerve (like the posterior tibial nerve) by around 5 msec using comparable stimulation sites (Burke, 1981 and Eisen, 1980). With mixed nerve stimulation, there is stimulation of both A-alpha cutaneous and Alpha motor neurons, which results in a shorter latency due to faster conduction speed of the fastest fibers stimulated.
So if we are stimulating nerve fibers that are both motor and sensory, the speeds at which they travel vary and will have a wider range. 70-120 m/s is the range often quoted (or above 50 m/s in the upper extremity and 40 m/s in the lower extremity is another general way it has been stated). It is this range of speeds that gives us the peak-to-peak duration.
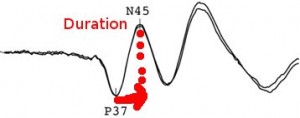
SSEP Onset-To-Peak Duration
When we look at the duration of a wave in a peripheral nerve, it’s usually one full cycle. This is representative of a traveling potential along the nerve, which has few outside influences. This takes into account the fastest to the slowest fibers contributing to the amplitude. The onset-to-peak duration of the cortical wave as depicted in the picture above only measures the area from the onset to the first turn. Unlike the full cycle duration, the onset-to-peak duration doesn’t represent the full spectrum of the speed of the conducting fibers, but gives us the best information for what we want to measure in our generator points.
Anyways, back to the original point being made…
As stated before, the rate of slowing that happens as we age past the second decade of life in the motor fibers is not as profound as in the sensory fibers. So yes, it is true that the absolute latency will be affected as the fastest motor fiber slows due to loss of myelination, or if the fastest firing axons are lost. But it’s the difference in the rate of slowing over the decades between the motor and sensory fibers that also adds to the variability of conducting speeds, by increasing the onset-to-peak duration and having a drop off in the number of fibers that fire at those predictive times needed when collecting an averaged response. The result is desynchronization.
And let’s face it, each fiber does not slow in a uniform fashion with the other fibers in that nerve. When slowing is reported as something like “0.4–1.7 m/s per decade,” it’s a range used to describe the general slowing in that population studied. If you took those numbers and applied it to an equation with some other known values (current speed of conduction, length of nerve recorded), you might come close to figuring the future latency. But that only tells you about the fastest fiber being stimulated. It’s not going to tell you about the conduction speed of the other fibers that make up that evoked response. Those ranges don’t necessarily represent all fibers being stimulated.
Masato Tanosaki found that it was not the increase in the onset as a major factor, but rather the increase in duration of the onset-to-peak.
Conclusion: Conductive function is affected by normal aging in the central as well as peripheral somatosensory pathways. The peak CCT (central conduction time) is more affected by aging than the onset CCT. However, the onset-to-peak duration of the N20–P20 increased by 0.8 ms between the 4th and 7th decades, suggesting that the peak CCT increase in older people reflects the age-related changes in N20–P20 profile but not in the fastest central conduction. We therefore conclude that the onset CCT measurement is preferable to the peak CCT measurement when assessing the central somatosensory conduction.
More reasons
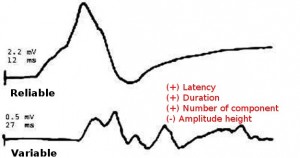
I’ve been concentrating mostly on the timing of the evoked potential, but there is more to it than that. There is also evidence of decrease in amplitude on CNAP testing. By age 60, the sensory CNAP amplitudes have dropped 36%, and by age 70 is half the size than it was at age 20. Since amplitude size is decreasing, we can assume that the number of axons viable has also decreased (since amplitude reflects indirectly the number of axons that can be activated). It might be the fastest fiber, it might be the slowest.
And of course, temporal dispersion itself has been measured. (LaFratt, 1966) demonstrated in nerves of 50-59 year old, there was a lower amplitude, increased duration, increased temporal dispersion and a higher number of components.
And as I said in my previous post, this is even more critical in the lower extremity with posterior tibial nerve stimulation at the ankle, especially the far-field subcortical response. Slow-conduction fibers lag behind faster conducting fibers over long conduction paths.
Wow this is getting long winded
There’s more to the story here, and I’ll continue this discussion in a later post. In my next post, I’ll show an example of what temporal dispersion looks like in a central lesion from a conduction block, and see if I can’t sum all this up.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
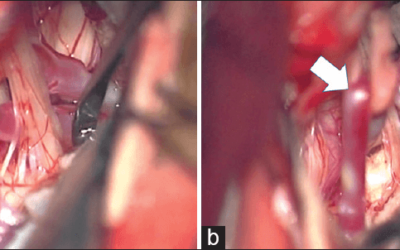
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
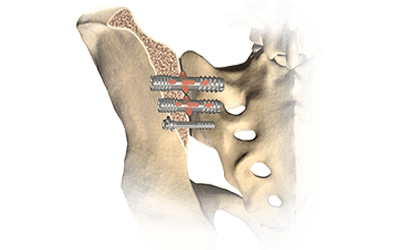
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...




hellow how are you joe?
I’m really glad to meet you even text
i am a Neurophygiolist in s.korea
and i working in Seoul National Hospital Neurosurgery department in korea
i working which intraoperative neruro monitoring at NS room
actually in korea, we can work Neuro part with medical technologist certification (MT)
I wanna work in United state with my IOM experience in korea,learn more good quality monitoring and contribute.
so i wanna have Qualityfy with ASNM to have certification
is there are for international people?
could you tell me about how to be ASNM neurophygiolist(intraoperative neuro monitoring,IONM))?
can i use my korea experience ?
sorry about my poor english mail
i hope to your response
HAVE A GOOD TIME
Hi Kimboeun. I’m sorry that I do not have an official answer for you, but you can find out more information here… http://abret.org/cnim/eligibility/
My guess would be that your cases are OK. You’ll just have to make sure you have all the requirements and pass the exam. I’d contact someone at ABRET (http://abret.org/resources/contact/) for an official answer. Hope it works out for you.