Optimizing Sub-cortical SSEP
There is 1 electrode that I see get misused in somatosensory evoked potentials more so than any other electrode in any modality. This is the electrode placed over the cervical spine (or sometimes around the ear or mastoid) and generally referred to “sub-cortical SSEP responses.” Surgical neurophysiologists use SSEP more than any other modality and the vast majority place this cervical electrode as part of their montage. For that reason, I think it is a worthwhile exercise to really dive deep into what is going on when we record SSEP from this electrode.
Why is there cervical electrode confusion in the first place?
I think the confusion is due to a couple of reasons.
- Far-field potentials are second class citizens in the operating room due to difficulty in acquiring them in an electrically hostile environment. For this reason, many of us have not devoted much time to understanding the generators of some of these potentials.
- Lesions that would unmask the differences are not common.
- We most likely understand what is creating the signal, but aren’t 100% sure.
So I am going to break down all the potentials that can be recorded using a needle in the neck. That means it can either be the active or reference electrode when stimulation comes from the upper or lower extremity. And since some people use this electrode anywhere from the lower cervical spine to the mastoid, I am going to include all potentials that we can collect from those areas.
The Upper Extremity SSEP
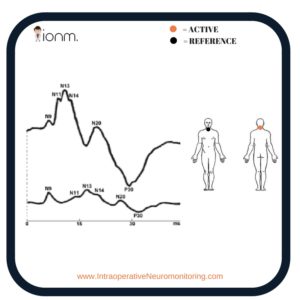
For the upper extremity SSEP, we are going to break down the following potentials: N9, N11, N13.
N9
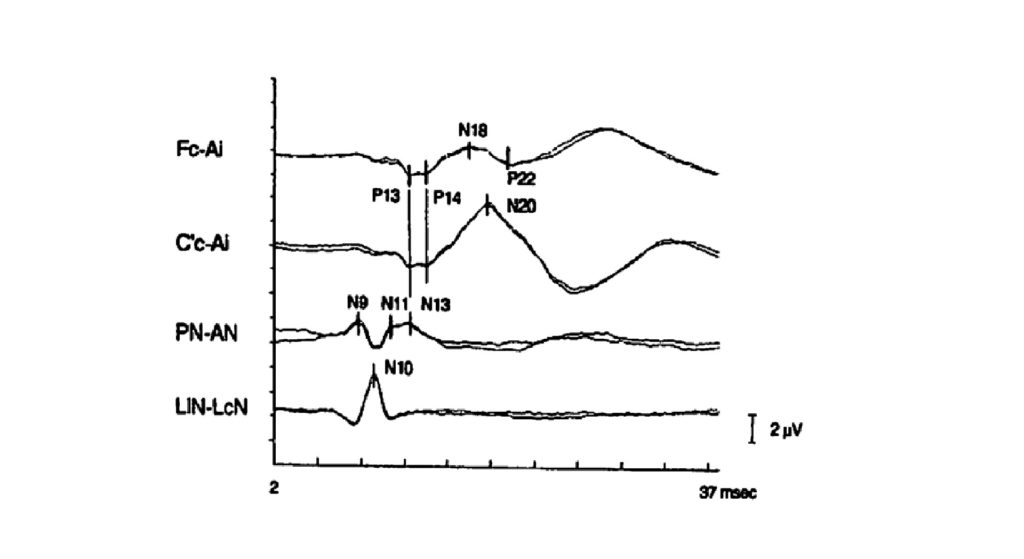
In order to record this response, a Posterior Neck – Anterior Neck setup is necessary. This N9 response is the same as the P9 response when the active electrode is placed over the head (FPz or CPz) and a distant reference electrode is used contralateral to the limb stimulated.
The contralateral knee and hand have been used successfully, whereas the P9 diminishes as the reference electrode moves closer to the head. This potential represents the distal brachial plexus.
Have you ever used it in the operating room?
Bonus CNIM material – This N9 or P9 far-field response is analogous to the P17 in the lower extremity.
N9 on Joe’s usefulness scale = 1/10
P11 and N11
The P11 is recorded from a scalp to non-cephalic derivation. When the lower cervical spine (Cv5) is referenced to a scalp electrode, the typically small far-field N11 potential is larger because of the additive P11 potential.
This N11 is the same thing as the P11 far-field response, just opposite in polarity due to the recording electrode over the posterior neck (which is what this post is all about).
It rides along the N13 hump and is thought to be presynaptic activity in the root entry zone and/or afferent volley transversing the dorsal cord (depends on the electrode placement… add another 1ms if as it passes up from the lower cord to upper cord, but still considered the N11).
It isn’t present in everyone, which makes it not very useful.
Have you ever used it in the operating room?
P11 and/or N11 on Joe’s usefulness scale = 0/10
N13 (Cv5 vs Cv2)
The N13 is a near-field response with a horizontal dipole. That means that it is more negative in the posterior neck, and more positive in the anterior neck. If it weren’t for the actual surgery, we might record from posterior neck – anterior neck.
There is no latency difference if the active electrode of the cervical response is placed over the spinous process of C5 or C2. For that reason, it is generally accepted to place the electrode at either location.
The practice of placing it in one position over the other without considering the case might not be the best practice.
Here’s why…
It is thought that the Cv5 location records the postsynaptic activity in the dorsal horn interneurons located close to the gray matter (this potential has been called N13a).
Patients with a syrinx impairing the pain pathways have had reported a loss of the N13a (Cv5) with an intact N11, N13b, P13/P14 and N20 response. This is because the other generators are reliant on the dorsal column medial lemniscal pathway (white matter), whereas N13a is the dorsal horn (gray matter).
This Cv5 can be more isolated from upper cervical and brainstem far-field responses by referencing it to a non-cephalic electrode (like Erb’s point). You’ll probably pick up those other earlier far-field responses coming from the brachial plexus and/or nerve roots.
Cv2 looks very similar to Cv5 in amplitude and latency, but most likely comes from completely different generators (has been called N13b). The origins of N13b (Cv2) seems to come from the dorsal column presynaptic activity at the cuneate nucleus.
We’ll talk about some scenarios later, but I think you should really consider the case at hand before sticking this electrode anywhere in the neck.
Have you ever used it in the operating room?
N13 on Joe’s usefulness scale = 10/10
PRO TIP: In cases like posterior cervicals, there is no law against recording from the positive end of the dipole and placing the electrode in the anterior part of the neck. Just keep it out of the view of Xray. Just something to consider in a pinch.
Lower Extremity SSEP
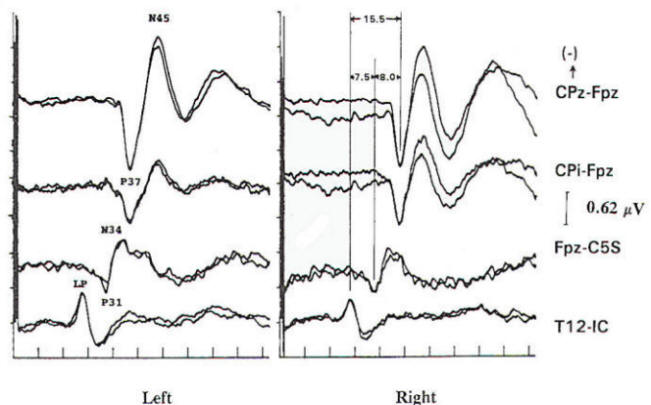
For the lower extremity SSEP, we are going to break down the following potentials: P31 and N34
I see 2 common misconceptions with this recording.
- This is sometimes called a cervical response, but there is no activity over the cervical spine coming from lower extremity SSEP. These potentials do not monitor the cervical spine. Do yourself a favor and call this a “sub-cortical SSEP” response. While you wouldn’t be wrong calling the upper extremity N13 a subcortical response, you’d be more descriptive if you called it a “cervical” response. Better clarity and makes things easy to remember.
- Since the cervical spine is inactive with lower extremity SSEP, you probably do not want an electrode recording from that area. There is activity over the scalp (more frontal area for N34), so that is a better anatomical location to record your response. The ears can also be used as a reference (eliminates some far-field responses) as well as the inactive neck. (Edit: I was reminded by Andrew Goldstein that we all have differential amplifiers, making the carryover of the “active” and “reference” electrode mean something different. The old EEG machines used a referential amplifier, so only 1 electrode was actually active. Differential amplifiers measure the voltage difference between the two signals at each of its inputs. For some reason, I seemed to forget that little fact mid-rant and needed to pay better attention when reading older studies like Erwin and Erwin’s Up and Down The Spine. But the main point still remains the same – the cervical spine is inactive in these lower extremity far-field potentials.)
The generators for these responses most likely come from multiple sources, with the P31 and N34 coming from the gracilis nuclei and/or medial lemniscus of the brainstem.
Have you ever used it in the operating room?
Joe’s grade: I would love if these were more reliable responses. These responses seem to go bad once temporal dispersion takes place. 8/10 – Lose points because the acquisition rate is less than desirable.
Let’s Make This Clinically Useful
Now that we’ve laid out some groundwork here, let’s see how we might use this clinically to better optimize our recordings and allow for more information to lend the surgeon with our differentials.
Case #1 – The patient presents with a C3/4 fracture. The surgeon doesn’t want tcMEP because of patient movement. He says he really has to rely on SSEP, so make it as good as you can. You have a lot of free channels to add additional recordings. Unfortunately, you work for a boss that doesn’t allow for anything outside of “his” protocols. If he gave you these 3 options, which one would you pick?
Case #2 – The patient is in screaming pain due to sciatica. The surgeon is going to do some decompression in the lumbar spine today but also has him scheduled for neck fusion in a couple of weeks. She lets you know that she is concerned about positional problems. Which seems like the most reasonable logic to you?
Case #3 – You’re assigned to a CPA tumor case, which is using BAERs already. Because of a lot of cranial nerves you’re monitoring, plus tcMEP in the facial muscles and extremities, you’re running low on available channels. Which seems to be the most reasonable thought process?
Case #4 – Anesthesia runs to your SNP in training and tells her that they need to run higher levels of the inhalational agent in this case… like 1.5MAC. The patient has a history of waking up in surgery a couple of times. This is an on a lumbar fusion with the only pertinent history is L4-5 radiculitis. You want her to come up with a reasonable game plan. Which response would you be most pleased with?
When I have a new surgical neurophysiologist in a case with me, I try to make it a point that (certain) subcortical waveforms can and should be used to provide more information. To use them only as a backup to cortical SSEP if anesthesia starts to take effect is incorrect.
You’ll either limit the amount of information you can relay to the surgeon should things go wrong, or incorrectly identify the level of the problem in certain circumstances (like the examples above).
I know they are not easy to get in the OR, but what’s your experience with them? Can you think of another example where a better understanding of the subcortical response can lead to improved outcomes?

Joe Hartman
Subscribe to our Awesome Newsletter.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...







0 Comments