SSEP P14 Potential: One Of The Unknown Obligates
Do you use a P14 potential for SSEP in the upper extremity?
I didn’t think so (don’t worry, I usually don’t either). But if you took a CNIM or DABNM exam, you’d think it would be a part of everyone’s montage. I mean, it’s an obligate peak, right?
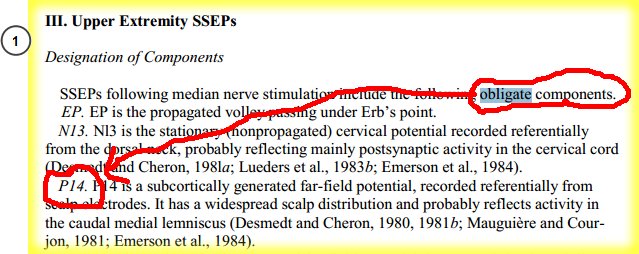
Obligate SSEP peaks include P14 potential according to the ACNS
The use of intraoperative somatosensory evoked potentials (SSEP) for the upper and lower extremities seems to vary from one group to the next.
And the confusion doesn’t stop with what’s happening in the field… the research isn’t much different. Some authors are in love with cortical SSEP potentials, so much so that they go on to say that subcortical responses might not even be needed. While other authors will take a subcortical response all day, because they know the effects anesthesia has on cortical SSEP waves. And I’m sure you already know my (waffling) opinion on if you should do a peripheral response for SSEP.
In upper extremity SSEP, I would say at the very least most groups are running a cervical and cortical response (probably 2 cortical channels). I assume that the majority are also using some sort of peripheral response, but I could be wrong about that as well. I really haven’t heard much about people using the far-field P14 recording, though it’s considered an “obligate” response by the ACNS.
So I figured I’d spend a little time going over the P14 response, for those looking to pass the DABNM or CNIM exam or those that might find it useful in certain scenarios.
The P14 Potential
The P14 potential is a far-field response that is believed to be around the level of the foramen magnum as the dorsal column is becoming the medial lemniscus (but could also include the cuneate nucleus). That means that the physiologic recordings are coming from either the propagation of action potential volleys in the medial lemniscus and/or the postsynaptic responses of the cuneate nucleus. And because this is a far-field response, we know that the generator points could be from changes in geometry (thickness) or conductivity of the volume conductor or change in direction of the nerve/tracts. That’s why the passing of these posterior tracts across the foramen magnum is one of the areas it’s assumed the waveforms are being generated.
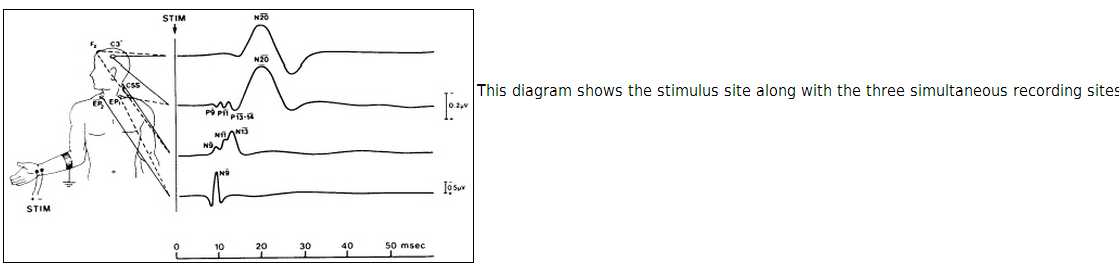
However, when you change your reference electrodes, you may change the amount of influence from the different generators, yet you still end up with a stationary response. In this far field potential (generators are far from the recording electrode, so small amplitudes), you have an active cortical (usually Fz or C3/4) and a non-cephalic reference (like the contralateral shoulder).
Let me repeat that last sentence, because there is often confusion in the field. You have an active cortical channel and a non-cephalic reference. Do not have an active electrode over your C5 spinous process and call this a cervical potential. It is not.
It may be a subcortical channel, but it the P13 has no recording over the cervical spine. If you are doing it this way, you probably see an inverted wave. This is not the optimal setup.
(NOTE: The use of a non-cephalic references can lead to large inter-electrode distances and pick up artifacts a little easier… probably the reason why the P14 isn’t a fan favorite.)
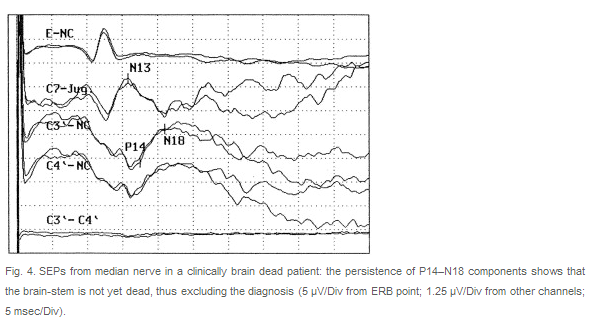
If you use an ear or nasopharyngeal reference, part of the area being recorded by the P14 response may be a little more rostral. For a thoracic case, this means next to nothing for us. But if you’re doing a case where cortical ischemia or possible brain death/coma is present, this little bit of info can help out. For instance, the Fz-Nasopharyngeal P14 potential is more rostral than the Fz-Contralateral shoulder P14. This set-up is absent in brain death, yet preserved in coma patients. It’s been shown that these P14 potentials are present in thalamic lesions (where scalp-scalp recordings were affected), but could not be recorded below the level of the foramen magnum.
Another important tidbit about recording a P14 response is that you use ipsilateral stimulation to the side recorded. So that would mean a left median stimulation could have a C3-R shoulder recording. In addition to the P14 wave, these far field set-ups can pick up other far-field recordings, like P9, P11 , and P13. But only P14 is an obligate wave.
Using The P14 Potential In The Operating Room
Congratulations to you if you’re still reading… especially if you do only intraoperative neuromonitoring! You can tell that this kind of information is probably better suited for those in the diagnostic world. I mean, how many times have you had to try to decipher brain death from coma during an c6-7 ACDF?
But could it be of value if it you were monitoring an odontoid fracture? Your N13 might be caudal to the surgical site, and N20 might be susceptible to anesthesia. Monitoring over the medial lemnisus in the brainstem could be of some use… no?
If you use this response or not, you’re probably still going to see questions from the diagnostic world on your DABNM and CNIM exams. The ACNS does still influence our field after all. So for those of you looking to take the exam, I hope this was a little more helpful than just putting P14, DCML, vertebral-basilar artery, far-field a couple other buzz words.
And for the rest of you… anyone monitor the P14 potential regularly? How reliable has it been for you? Has it helped in any specific cases you’ve done?
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
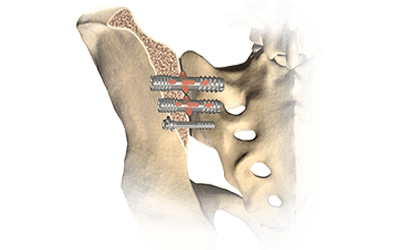
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...