The Popliteal Fossa Response
I got an email the other day for someone looking for some help with obtaining a popliteal fossa potential…
Joe,
Thanks again for the help! Had a question… with the Pop Fossa, what montage do you use for it? I’ve never done them, nor been trained/taught how to get them and looked through 3 references and cannot find info on obtaining them.Thank you!
A Little Background Info
Set-Up The Popliteal Fossa Potential
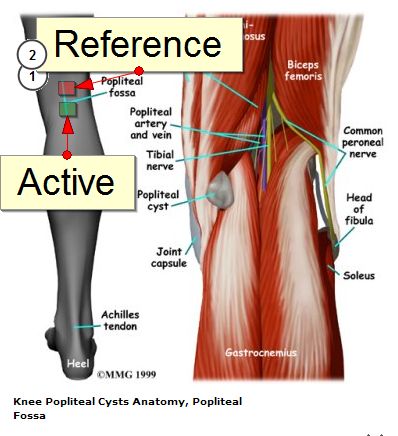
Here’s a quick video on the anatomy of the popliteal fossa. Notice the surrounding muscles and how poor placement of the electrodes could cause recording problems.
- Gain: 10 uv/div
- HiCut: 300
- LowCut: 30
Troubleshooting Popliteal Fossa Response
Since this is a response that is directly over the nerve before any synapses, you should get a response in most of your cases. Here’re some things to try if you’re not getting a reliable response.
- Check to make sure you are plugged in correctly. Switching a left for a right is going to totally eliminate your response.
- Make sure your placement is over the tibial nerve. By the time it’s traveled up the medial aspect of your lower leg, it becomes pretty midline as it joins the common peroneal nerve to make up the sciatic nerve. That’s where your best window of recording over the nerve is located. The heads of the gastrocnemius, semimembranosus, semitendinosus, biceps femoris and popliteus muscles make up the border of the popliteal fossa, but also serve as a pretty good barrier. Lower your resistance by avoiding being over these muscles.
- Change from a surface to needle electrodes. Sometimes people have swelling or fat deposits that can hamper your recordings. Going subcutaneous can help eliminate some of that.
Precautions
Besides the universal precautions, you need to work with the nurse in the room with the placement of the bovie pad. The electric cautery will shunt current, and it will travel the path of least resistance. If it happens to travel to your electrodes (especially the subcutaneous needles), this could cause a burn injury to the patient. While this is possible at any electrode you place on the body, I’ve noticed it more here than anywhere else. You’ll want the nurse to place the pad up high in the back of the thigh/buttock (yet still out of the field) and not over a hairy patch of skin. They may need to shave them. The placement of the pad is their job, so only make them informed of the possibility of the burns and what seems to work best.
Clinical Use
Just like Erb’s point, the popliteal fossa potential is useful as a peripheral response to verifying that there are no technical problems from the machine to the nerve. If you can record a pop fossa response, then you know you have good electrical output.
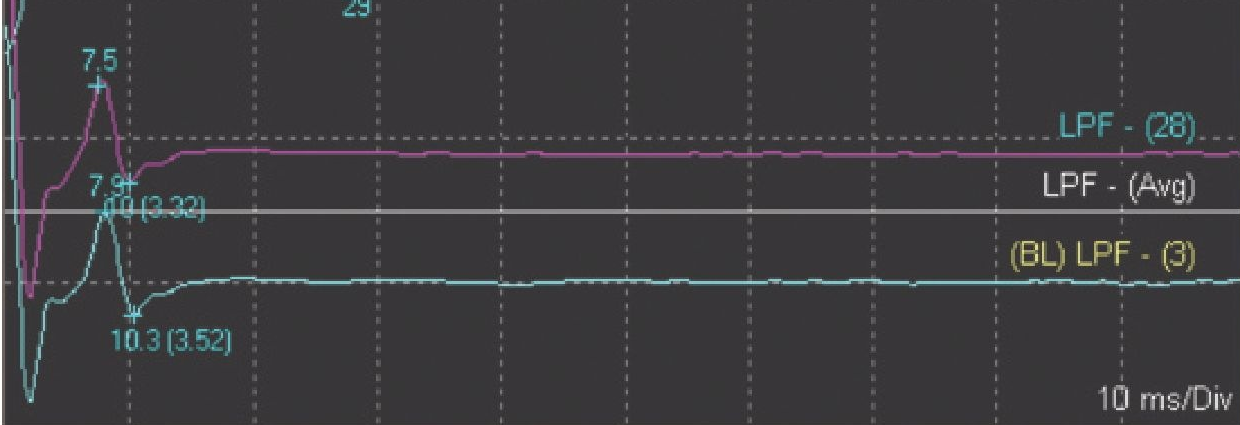
It can also be used to determine the amount of stimulation to use. Some use the “twice motor threshold” (or about 6-10 mA X2) to set their stimulation while others might just shock the hell out of them (still within the guidelines, of course). Instead of just cranking up the juice, you can tell how high you turn up your simulator by watching your pop fossa wave. When its amplitude stops increasing, you have met the maximal threshold.
Practice, Practice, Practice
When I was doing electrodiagnostic studies, I had the opportunity to zap a bunch of different nerves on a bunch of different people with NCV testing. I was able to get immediate feedback if I was on the nerve or not. It is a little bit harder to get that direct feedback in the OR, and I think most of us take the lazy route of increasing the stimulation intensity or pulse duration for our SSEPs. For those that have had to train without this type of feedback, there’s still a place to learn for free. It’s called youtube. Here’s a video showing stimulation sites in multiple areas. It might help you better understand where to stimulate to get something like a popliteal fossa response.
Closing Thoughts
The popliteal fossa potential is an obligate point, and you should be running it. Besides the information it gives you and proof that there is no technical error in stimulation, if you get called to court for the case (or use it on the DABNM exam), you will wish you had it there.
In the long run, could you run your cases without a pop fossa response and still have the same overall outcomes? Probably. Especially since most machines will tell you if there is a stimulation problem or not. But it’s not worth the risk, so CYA.
What do you think? Are you using them? If not, did I change your mind?
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...