SSEP Baseline
One of the few things in IONM that’s agreed upon (well, mostly anyways), is that an amplitude reduction of 50% in SSEP baseline, or a 10% latency shift off of those somatosensory evoked potential baselines, is a reliable alarm criterion to use during surgery.
But as we all know, the first trace taken can vary from the second. The second from the third. And certainly the third trace compared to one taken 1 hour later.
So when should we set our SSEP Baselines?
I’ve talked with some people who like to take a look at the first couple of traces and assess if there is much variability between the traces. If there isn’t, then they’ll set their baselines right there and leave it the remainder of the case. If there is some variability, they’ll continue to collect pre-incision traces and set the baseline when it falls somewhere in the “average” range (Of course this is all assuming that technical troubleshooting has done as much as possible to eliminate interference).
Others will set an initial baseline, and “wait and see.”
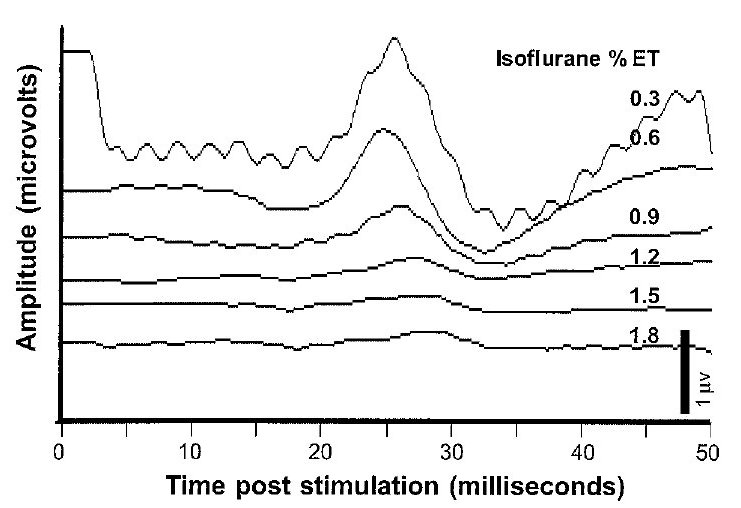
While I’m in the second group myself, you still need to be able to know how long you can actually wait till you set a final SSEP baseline. We know that anesthetic effect on synapses and temperature changes on conduction speeds can have a gradual change throughout the case.
Using reason, it seems like a good idea to have your baselines set at a time where the patient’s body has had time to adapt to the surgical environment, but still soon enough that you aren’t misinterpreting neurological compromise as a gradual change. That makes me think that setting baselines at some point during the case where neurological compromise is not probable, like removing a bone flap during a craniotomy.
But I also like science to back up or verify my reason, so I was glad to read this study done by Chen, 2004…
Variability of Somatosensory Evoked Potential Monitoring During Scoliosis Surgery
Results: We found the latency showed a significant increase and the amplitude significant reduction from stages 1 to 2. There was no significant variability from stages 2, 3, and 4, but both latency and amplitude recovered significantly from stage 4 to 5. [The authors defined each of these stages in accordance to scoliosis surgeries, but you can adapt the timing and logic to other surgical procedures since we still have the same concerns about appropriate SSEP baseline measures. Stage 1 was is pre-incision. Stage 2 exposure. Stage 3 is instrumentation. Stage 4 is deformity correction. Stage 5 is wound closure] This variability correlated with the changes in mean arterial pressure and end-tidal concentrations of isoflurane and was not dependent on the type of surgical procedure. If either 50% amplitude reduction or 10% latency prolongation of SSEP compared with baseline recordings at stage 1 (pre-incision) was used as warning criterion, the overall false-positive rate was 23.1%. It was significantly reduced to 7.7% if stage 2 (spine exposure) recordings were used as the baseline (P ). The false-positive rate decreased to 0% if a combined 50% amplitude reduction and 10% latency prolongation of SSEP compared with the stage 2 baseline were used [This is very important to note. Just by taking a correct SSEP baseline, they improved to a specificity of 100% in their sample. People ask me why I have a blog… why help train the competition? It’s because it is in all our interest to increase awareness. Patients won’t get the care they deserve, surgeons will stop using test they can’t rely on, insurance companies will stop paying for something that isn’t cost effective, etc. all because of poor monitoring. Overall, someone making this mistake hurts the reputation of the field. For example, here’s a presentation that talks about a higher rate of false positive SSEP with scoliosis correction on slide 31/50. When I see claims like this, I’d like to see what their experience has been to lead them to this conclusion.]
Conclusion: Based on these findings, we concluded that the time to obtain SSEP baseline data should be adjusted to post incision instead of pre-incision.
Great! I know I have some scientific backing to my reasonable hunch.
But of course, it’s not always that easy. I’ll go over some other scenarios in a later post where choosing SSEP baselines aren’t always so clear.
Until then.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...