The Trapezius Muscle In Intraoperative Neuromonitoring
If we follow the same medical textbooks we used in school to pass a test, then we know for sure that the motor portion of the trapezius is innervated by the spinal accessory nerve (CN 11) and the sensory portion is from C2-4. In clinical practice, things may not be so simple.
There still remains controversy over the innervation makeup of this muscle. This most likely stems from the fact that there are variations in findings due to different research methods and the assumption that there is a poor understanding of the actual anatomy. We’ll go through some of the findings in the literature and then apply it to neuromonitoring.

Innervation To The Trapezius Muscle
In multiple studies (like Faherer, 1974 and Petrera, 1984), there was a very high rate of stimulation of all 3 parts of the trapezius muscle when stimulating the main trunk of the spinal accessory nerve. I don’t think most people would consider those finding surprising. Nor would most argue that the main contribution of motor function comes from those fibers.
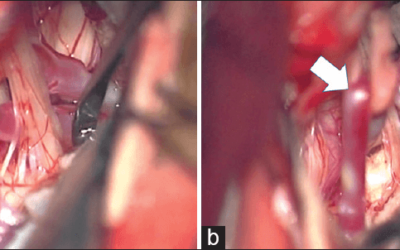
But what should be noted is that if this nerve is dissected (as seen in the posterior triangle during surgery or even some suspect this can happen in some whiplash injuries), you will see an uneven distribution of weakness seen clinically. The upper trapezius is usually affected greater than the lower muscles. It should also be noted that these motor fibers from the cervical nerve roots can also supply the entire trapezius muscle, so weakness can be seen more evenly distributed.
In addition to clinical findings, there are studies that have shown CMAPs with direct electrical stimulation of the cervical nerve roots.
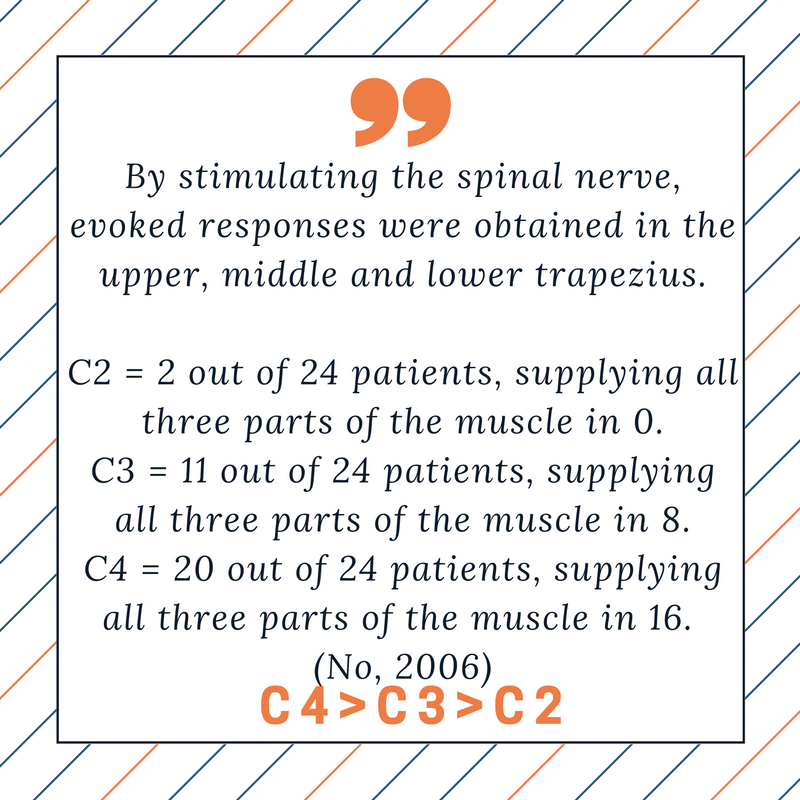
But what about studying the nerve root themselves? If you cut the C2, C3 and C4 nerve roots, what type of nerve fibers would you find? (Tubbs, 2011) performed an immunohistochemical analysis of fibers on cadavers. They found the presence of motor fibers at all levels, with C4 greater than C3 and C3 greater than C2.
Monitoring The Trapezius Muscle During Surgery
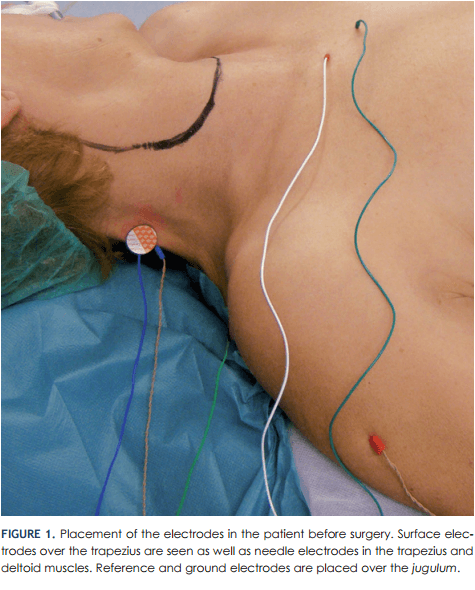
Notice the surface electrode. Their claim is that it captures a wider space of muscle activity vs the needle electrode. The Skinner paper would disagree with this technique.
Due to the possibility of multiple nerve roots + the spinal accessory nerve supplying motor function in varying amounts and varying in sections of the muscle, it becomes very difficult to speak in any sort of absolutes, like: “I am using the trapezius muscle as an MEP control in the C3-7 spine surgery,” or “I am able to effectively monitor the motor portion of C3 by using the trapezius for EMG monitoring.”
But we may be able to adjust our setup to give us better odds. And knowing about these clinical shortcomings can help better make sense of aberrant findings as they compare to what is happening surgically.
Here are some suggestions:
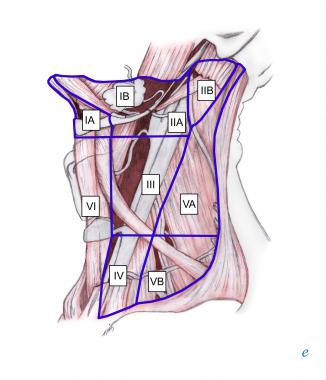
- Place your electrodes in the upper trapezius if you are looking to monitor the spinal accessory nerve during cranial nerve monitoring, or utilize the trapezius muscle as a control for MEPs during cervical surgery.
- Reference your electrodes in the middle and lower trapezius if using the trapezius to monitor the nerve roots with EMG.
- Understand the probability of innervation for each segment of the trapezius and level of the cervical nerve roots. This may help you give better differentials to the surgeon should something not fit a “textbook” finding.

Joe Hartman
Subscribe to our Awesome Newsletter.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
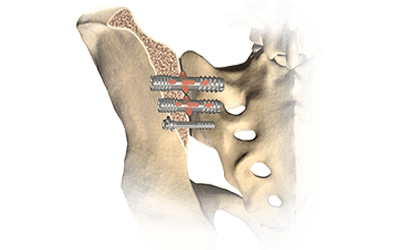
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...




0 Comments