When talking about intraoperative monitoring of visual evoked potentials, it’s almost like you’re getting a history lesson, seeing as most groups aren’t doing them. And most have 2 things that come to mind right away.
First, visual evoked potentials have been used for pituitary surgeries.
Second, visual evoked potentials don’t really work well in the operating room.
It’s pretty well-known that anesthesia just eats visual evoked potentials right up. It’s too bad, because when you practice VEP on your non-anesthetized buddy, that P100 amplitude seems pretty stable.
During one of my pubmed searches to see what’s new, I ran into this article…
Continuous monitoring of cortical visual evoked potentials by means of subdural electrodes in surgery on the posterior optic pathway. A case report and review of the literature.
Torres CV, Pastor J, Rocio E, Sola RG.
Source Hospital Universitario de la Princesa, 28006 Madrid, Espana.
Abstract
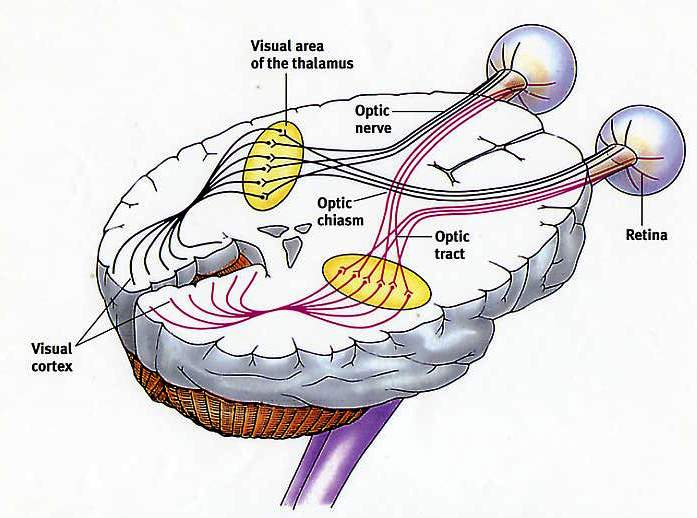
INTRODUCTION. Intraoperative monitoring of functional language and motor areas is a commonly used technique which makes it possible to minimise the post-operative sequelae and to perform an optimal resection of lesions in these areas. Monitoring of the visual cortex, however, is not usually carried out nowadays. The scarce spatial resolution and its sensitivity to anaesthesia are some of the technical difficulties that reduce its clinical usefulness. The study reports a case of resection of an occipital lesion under general anaesthetic, with intraoperative monitoring of the cortical visual evoked potentials (VEP) by means of subdural electrodes.
CASE REPORT. A 50-year-old female who underwent surgery involving the resection of an occipital lesion that was suggestive of radionecrosis. The VEP were monitored by administering flashing light at 4.1 Hz and recording with subdural strip electrodes on the occipital cortex. During the operation, a progressive lowering of the amplitude of the cortical VEP was observed when 50% of the baseline amplitude was exceeded, and thus the resection was finished. The increase in latency was below 10% of the baseline value. The patient recovered well during the post-operative period and her sight did not present any changes with respect to the baseline values.
CONCLUSIONS. In our case, monitoring the cortical VEP by cortical recordings produced stable recordings with a good correlation with the post-operative visual function. Cortical recordings performed either directly or by means of subdural electrodes make it possible to achieve adequate spatial resolution and response intensity. Further studies need to be conducted with a greater number of patients in order to obtain decisive conclusions.
Obvious more testing is needed, but this is a very interesting twist. I’ve seen similar cases posted at the hospital, but never felt like there was anything to offer.
Things to consider going forward…
- Will this prove to be more stable than visual evoked potentials with regular subdermal electrodes? Some people I’ve talked to that have done more than a handful of VEP say that it seems to be more reliable than what the literature indicates, but still has a high failure rate compared to SSEP monitoring. Maybe they got lucky the first couple of times and this will prove to be a bust. Remember, just because we can record a wave, doesn’t mean it gives it anything useful.
- What does it actually mean when there is a 50/10 change in VEP for this case. I’m not sure you can jump to the conclusion that these reductions are exactly like one’s seen with surgeries at the pituitary. Cortical tissue vs nerve tracts. Might be a leap of faith that needs more study.
While I still remain skeptical till more proof is published, this may end up being another useful service IOM can provide for surgeons and patients.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...