DABNM Prep Strategies – Answering “Why” and, “Says Who?”
One of the challenges faced by those taking on a DABNM question is that you not only have to be able to answer “why,” but also “says who.” That ends up being a lot of information to cram in there.
One suggestion I’ve given to those going through their DABNM prep is to look for more than 1 way to fit an answer to a question asked, or to use as an example in addition to another answer to building your case. You might be able to stretch out what you know over a greater range of DABNM questions if you’re able to adapt it to the situation.
Let’s look at an example.
Here’s what you have ready as an answer for “why” and “says who.”
“(Holland 1997) Showed EMG can pick up nerve root irritation where SSEP did not.”
DABNM question to apply it to:
- Why did you use EMG in this lumbar case instead of just SSEP?
- (Gunnarsson 2004) For peripheral nerve damage, EMG was 100% sensitive and 23.7% specific, while SSEPs are 28.5% sensitive and 94.7% specific. + (Holland 1997) showed EMG can pick up nerve root irritation where SSEP did not.
- What would you say to an insurance company that denies claims in an L4/5 PSF?
- Using both EMGs and SSEPs have been shown to be sensitive and specific for determining neurological insult in this type of procedure. Changes in spinal cord signals have been successfully identified by SSEP (Balzer, 1998). + (Holland 1997) showed EMG can pick up nerve root irritation where SSEP did not. Sala 2007 showed that even though the rate of neurological complications is low, neuromonitoring has decreased these rates even greater. With the high cost of care needed after neurotrauma from spinal surgery, the cost of intraoperative monitoring is more than justifiable.
- Would you consider using tcMEP to monitor peripheral nerves?
- As part of a multimodality approach = (Lyon, 2008) showed that traction on a nerve root does not always show corresponding EMG, yet does show some decline in MEP responses. + (Holland 1997) Showed EMG can pick up nerve root irritation where SSEP did not, which we would most likely see in tcMEP as well due to multiple root innervation.
Do you need to reference every answer you give? Of course not. But if the DABNM question being asked refers to exactly why you did something, it really helps to build your case and show your understanding of the literature.
A Second, More Creative Way To Think About Answering A DABNM Question
But I’d like you to try it the other way around. Here you’re coming up with an answer, and it can be pretty vague, and then applying different scenarios to that single answer.
Here’s the vague answer you’re going to apply your IONM knowledge to…
“Because sometimes in neuromonitoring, size matters…”
That’s all I’m giving you. Try to work with that initial answer.
This is just a mental exercise to try to cover as much ground as possible and come up with stupid ways to help things stick in your brain. Coming up with scenarios meeting a given criteria is just one way to do it.
For the sake of practice, I’m going to give you 5 instances where being LARGE in size matters.
Signal-to-noise ratio – We Want HUGE Signals
We’re always looking to increase the size of the amplitudes for evoked responses we are collecting. There are 2 main reasons for this.
First, the larger the amplitude, the more likely we are activating all the axons at the stimulation site. If we are not stimulating at a level that activates all the axons, then our postoperative outcomes may not match our recordings (for most modalities).
For instance, let’s assume that we are able to record a reliable somatosensory evoked potential with the stimulation site at the posterior tibial nerve and the recording site at CPz-FPz. The amplitude of this response is 0.4uV. But if the intensity was increased by 10mA, the response would have been 1.0uV. During the case, there was a conduction block of 50% of the axons due to a problem. Can you see how there might be a false-negative response if the axons lost did not make up the at least 50% of the axons activated during submaximal intensity? At the same time, can you also appreciate the risk for a false-positive response if a conduction block to a larger percentage of the axons used to create the 0.4uV response?
Second, the larger the amplitude of the evoked response, the better the signal-to-noise ratio will be. Not only does this make for easier interpretation, but also allows us to collect response quicker.
Say that the background noise overlaying your SSEP recordings is EEG activity + EMG activity + noise from the room, and that has an average height of 50uV. In the first instance, our lower extremity SSEP was 0.4uV in amplitude. That gives us the following:
Signal-to-noise ratio = (Signal amplitude)/(Noise amplitude)
= (0.4uV) / (50uV)
= 0.008
From here, we need to find the suppression factor, or the multiple used to bring the results of the signal-to-noise ratio back to 1.
1 = (0.008)*(√N)
√N=125
N = 15,625
What if we looked at the same equation with supramaximal intensity stimulation, resulting in an averaged response of 1.0uV in amplitude.
= (1.0uV) / (50uV)
= 0.02
Suppression factor
1 = (0.02)*(√N)
√N = 50
N = 2,500
Those averages are far higher than what we’re used to seeing, but it was used for the purposes of simple math and to illustrate the importance of signal optimization (similar examples found in Daube’s Clinical Neurophysiology book). Optimization includes using the best stimulating, recording and filtering practices.
Pedicle size – Give me a fat pedicle with strong bone.
When a surgeon drives a pedicle screw down into the pedicle of the vertebrae, he or she is hoping to see nice, large pedicles. Not only will they be less likely to misplace the screw, but the hardware should be less likely to fail over time.
The size of the pedicle also has a direct bearing on the threshold levels we use for our alarm criteria during pedicle screw stimulation. Just take the thoracic spine vs the lumbar spine for instance. The thoracic spine has much smaller pedicles when compared to the lumbar vertebrae. So that should help you better understand why currently accepted pedicle screw stimulation in the thoracic spine is 6mA and 8 mA in the lumbar spine.
It is also beneficial to know that L5 tends to be the largest vertebrae and S1 tends to have smaller vertebrae. So if you’re stimulating pedicle screws in the lumbar spine and get 9mA for 5 other levels and 7mA at S1, you should inspect the segment for a breach, but not be surprised if one is not found.
Longer intramuscular needles mean larger amplitudes in hard to reach muscles
Before I get into this optimization tip, I have to admit that I’ve never done a case with these longer EMG electrodes. I just never had the opportunity. Most likely it was cost as the main factor.
In theory, these electrodes might come in handy for certain muscle groups (mostly proximal muscles) in certain patient populations (large adipose tissue). I really doubt there is any difference in monitoring the first dorsal interosseous muscle, but I would be interested in seeing some side-to-side comparisons of rectus femoris or abdominal EMG and tcMEP responses over at least 100 random cases.
Here’s a nice video showing the possible value of having these longer electrodes intramuscular instead of subcutaneous.
MEP Stimulating Electrodes – Corkscrew electrodes for tcMEP INCREASES surface area to lower impedance
This on I’m on the fence about. There is evidence that using the corkscrew electrodes is superior to cup electrodes and subdermal straight electrodes due to lower impedance values with the larger surface area of the stimulating electrode.
I’ve used corkscrew electrodes for tcMEP for about 2 years and straight subdermal electrodes the remainder of the time. I can’t say that I’ve noticed much difference in my own observations. I could be incorrect in my unscientific assumptions, but I feel I have more control over finding the best production of tcMEP with the lowest amount of patient movement when I can adjust the head leads. Straight needle electrodes make this easier with less tissue damage.
2 questions that I’ve asked myself after coming to this conclusion:
- Could I achieve the same thing using corkscrew electrodes and still gain the advantage of lower impedance? Probably. But like I said, the difference, in my opinion, was not worth the additional trauma/bleeding I’ve notice from corkscrew electrodes.
- Would I be better off just using a lot of electrodes to cover those areas of the scalp instead of repositioning them? Is infection a concern? Again, I have no real data to back this up, but with the risk of infection being so low, and being careful not to bring the needle into contact with anything else but the patient’s own skin, I believe the risk to be close to non-existent. What I have seen is when I load the head up with electrodes, there is some shunting that can happen when I run a tcMEP. That’s no good.
Give me a HUGE MCA artery for TCD, please.
I’ve been battle tested when setting up TCD for CEA. I love it when the patient has an easy setup. Some patient populations are known to be more difficult due to a thicker bone through the temporal window (females, Asian and African ancestry). It is also well documented that artery size of all structures of the circle of Willis can vary in size.
I was always so happy to find a good, strong TCD trace from the ipsilateral MCA right off the bat. There are cases where the window is so small that any small perturbation of the probe will cause the response to disappear. It can be very frustrating.
There you go. 5 neuromonitoring scenarios where size matters. Nothing really all that similar, but bridging topics together like this has been used by people who teaching memory strategies. Maybe it works for you to answer a DABNM question?
How about a time when we prefer to have something small in size? Let’s see what you can come up with in the comments section.

Joe Hartman DC, DACNB, DABNM
Vice President Of Clinical Services - Sentient Medical
Want new articles before they get published?
Subscribe to our Awesome Newsletter.
Keep Learning
Here are some related guides and posts that you might enjoy next.
How To Have Deep Dive Neuromonitoring Conversations That Pays Off…
How To Have A Neuromonitoring Discussion One of the reasons for starting this website was to make sure I was part of the neuromonitoring conversation. It was a decision I made early in my career... and I'm glad I did. Hearing the different perspectives and experiences...
Intraoperative EMG: Referential or Bipolar?
Recording Electrodes For EMG in the Operating Room: Referential or Bipolar? If your IONM manager walked into the OR in the middle of your case, took a look at your intraoperative EMG traces and started questioning your setup, could you defend yourself? I try to do...
BAER During MVD Surgery: A New Protocol?
BAER (Brainstem Auditory Evoked Potentials) During Microvascular Decompression Surgery You might remember when I was complaining about using ABR in the operating room and how to adjust the click polarity to help obtain a more reliable BAER. But my first gripe, having...
Bye-Bye Neuromonitoring Forum
Goodbye To The Neuromonitoring Forum One area of the website that I thought had the most potential to be an asset for the IONM community was the neuromonitoring forum. But it has been several months now and it is still a complete ghost town. I'm honestly not too...
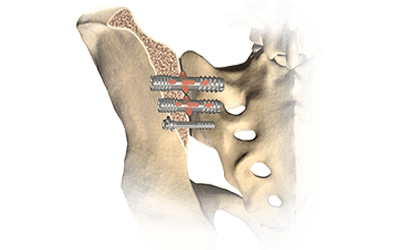
EMG Nerve Monitoring During Minimally Invasive Fusion of the Sacroiliac Joint
Minimally Invasive Fusion of the Sacroiliac Joint Using EMG Nerve Monitoring EMG nerve monitoring in lumbar surgery makes up a large percentage of cases monitored every year. Using EMG nerve monitoring during SI joint fusions seems to be less utilized, even though the...
Physical Exam Scope Of Practice For The Surgical Neurophysiologist
SNP's Performing A Physical Exam: Who Should Do It And Who Shouldn't... Before any case is monitored, all pertinent patient history, signs, symptoms, physical exam findings and diagnostics should be gathered, documented and relayed to any oversight physician that may...




0 Comments